Association of estimated glucose disposal rate with all-cause and cardiovascular mortality in individuals with cardiovascular-kidney-metabolic syndrome: Two prospective cohorts
IF 5.9
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
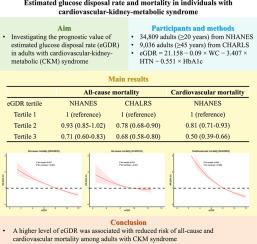
Given evidence on cardiovascular disease (CVD) risks conferred by comorbidity risk factors, the American Heart Association (AHA) introduced a novel framework, named cardiovascular-kidney-metabolic (CKM) syndrome. Accumulative evidence suggested that the estimated glucose disposal rate (eGDR) was significantly associated with mortality risk. However, it remains unknown whether this association exists in individuals with CKM syndrome. This study aimed to investigate whether eGDR can predict all-cause and cardiovascular mortality risks among adults with CKM syndrome.
Methods
This study used data from two prospective cohorts: the National Health and Nutrition Examination Survey (NHANES) and the China Health and Retirement Longitudinal Study (CHARLS). The exposure was eGDR at baseline, which was calculated using a combination of waist circumference, hypertension, and hemoglobin A1c. Cox regression models and restricted cubic splines were used to calculate the hazard ratio (HR) and 95 % confidence interval (95 % CI) after adjusting for potential confounders. The main outcomes were all-cause and cardiovascular mortality.
Results
A total of 34,809 participants (female: 50.8 %, mean age: 46.7 years) and 9,036 from CHARLS (female: 53.3 %, mean age: 59.6 years) were included. The median follow-up periods were 8.3 years in NHANES and 9.0 years in CHARLS. Per 1-SD increase in eGDR was associated with 18 %-24 % lower risks of all-cause mortality after adjusting for confounders (NHANES, HR 0.76, 95 % CI 0.71-0.82; CHARLS: HR 0.82, 95 % CI 0.77-0.88). In NHANES, the adjusted HR (95 % CI) for per 1-SD increase in eGDR was 0.60 (0.53–0.68) for cardiovascular mortality. The dose-response curve between eGDR and mortality risks showed a negative linear relationship in individuals with CKM syndrome.
Conclusion
A higher level of eGDR was associated with reduced risk of all-cause and cardiovascular mortality among adults with CKM syndrome. eGDR can serve as a promising predictor and therapeutic target for reducing mortality risks among CKM adults in clinical practice.
心血管-肾代谢综合征患者估计葡萄糖处置率与全因死亡率和心血管死亡率的关系:两个前瞻性队列
背景:鉴于心血管疾病(CVD)风险与合并症风险因素相关的证据,美国心脏协会(AHA)引入了一个新的框架,称为心血管-肾-代谢(CKM)综合征。累积的证据表明,估计的葡萄糖处置率(eGDR)与死亡风险显著相关。然而,这种关联是否存在于CKM综合征患者中尚不清楚。本研究旨在探讨eGDR是否可以预测成人CKM综合征的全因和心血管死亡风险。方法本研究采用两个前瞻性队列的数据:国家健康与营养调查(NHANES)和中国健康与退休纵向研究(CHARLS)。暴露量为基线时的eGDR,结合腰围、高血压和血红蛋白A1c计算。在调整潜在混杂因素后,使用Cox回归模型和受限三次样条计算风险比(HR)和95%置信区间(95% CI)。主要结局为全因死亡率和心血管死亡率。结果共纳入34809例(女性50.8%,平均年龄46.7岁)和CHARLS 9036例(女性53.3%,平均年龄59.6岁)。NHANES的中位随访期为8.3年,CHARLS的中位随访期为9.0年。校正混杂因素后,eGDR每增加1 sd,全因死亡风险降低18% - 24% (NHANES, HR 0.76, 95% CI 0.71-0.82; CHARLS: HR 0.82, 95% CI 0.77-0.88)。在NHANES中,eGDR每增加1 sd,心血管死亡率的校正HR (95% CI)为0.60(0.53-0.68)。CKM综合征患者eGDR与死亡风险的剂量-反应曲线呈负线性关系。结论高水平的eGDR与CKM综合征成人全因死亡率和心血管死亡率降低相关。在临床实践中,eGDR可作为降低CKM成人死亡风险的一个有希望的预测指标和治疗靶点。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

American journal of preventive cardiology
Cardiology and Cardiovascular Medicine
CiteScore
6.60
自引率
0.00%
发文量
0
审稿时长
76 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


