Early detection of antiseizure medication inefficacy using an implantable continuous EEG system and a personalized model: a case study
IF 1.5
Q3 CLINICAL NEUROLOGY
引用次数: 0
Abstract
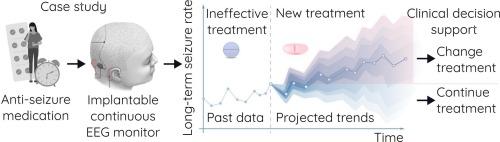
Evaluating anti-seizure medication (ASM) efficacy can be limited by inaccurate seizure diaries and periodic fluctuations in seizure frequency, known as seizure cycles. These limitations may prolong monitoring of ineffective treatments. This study explores implantable continuous EEG monitoring (iCEM™) with Epiminder’s Minder® system and timeseries modelling to improve efficacy assessments.
This retrospective case study examines a 49-year-old female with drug-resistant focal epilepsy with iCEM (Nov. 2019). The participant maintained a seizure diary and was followed-up for 3 years. ASMs were changed in Aug.-Oct. 2020. A personalised autoregressive model incorporating interictal epileptiform discharge cycles to project 3-monthly seizure rates was trained and validated on post-drug data then tested on four held-out datasets (two pre-drug and two post-drug). The Kruskal-Wallis test assessed model performance between drug periods (α = 0.05).
Only 37 % of seizures were reported. Post-drug, diary-reported seizures increased while detected seizures decreased, but both remained within normal seizure rate variability. ASM inefficacy was addressed after 3 years. The autoregressive model mean squared error post-drug was 0.17 and 0.13 seizures per day over 3-months2, which were significantly different from pre-drug (0.49 and 0.58 seizures per day over 3-months2, =336.82, p = 2.44exp.-89), suggesting the model could recognise when an altered drug regimen affected seizure rate and interictal epileptiform discharges.
Seizures identified using iCEM combined with an individualised model may be able to distinguish drug-induced changes in seizure rate from normal variability. This proof-of-concept study offers useful information towards the development of methods that can support early treatment assessments, potentially shortening the time to find an optimal therapy.
使用可植入连续脑电图系统和个性化模型早期检测抗癫痫药物无效:一个案例研究
评估抗癫痫药物(ASM)的疗效可能受到不准确的癫痫发作日记和癫痫发作频率的周期性波动(称为癫痫发作周期)的限制。这些限制可能会延长对无效治疗的监测时间。本研究利用Epiminder的Minder®系统和时间序列模型探索植入式连续脑电图监测(iCEM™),以改善疗效评估。本回顾性病例研究对一名49岁耐药局灶性癫痫女性患者进行了iCEM检查(2019年11月)。患者记录癫痫发作日记,随访3年。8月至10月,asm发生了变化。2020. 一个个性化的自回归模型结合癫痫样放电周期来预测3个月的癫痫发作率,在药物后数据上进行训练和验证,然后在四个固定数据集(两个药物前和两个药物后)上进行测试。Kruskal-Wallis检验评估各给药期模型性能(α = 0.05)。只有37%的癫痫发作被报道。服药后,日记报告的癫痫发作增加,而检测到的癫痫发作减少,但两者都保持在正常的癫痫发作率变异性范围内。3年后ASM无效。用药后的自回归模型均方误差分别为0.17和0.13次/ 3个月2,与用药前的0.49和0.58次/ 3个月2差异有统计学意义,H=336.82, p = 2.44exp。-89),这表明该模型可以识别出改变的药物治疗方案何时会影响癫痫发作率和发作间期癫痫样放电。使用iCEM结合个性化模型识别癫痫发作可能能够区分药物引起的癫痫发作率变化和正常变异性。这项概念验证研究为开发支持早期治疗评估的方法提供了有用的信息,有可能缩短寻找最佳治疗方法的时间。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Epilepsy and Behavior Reports
Medicine-Neurology (clinical)
CiteScore
2.70
自引率
13.30%
发文量
54
审稿时长
50 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


