MELD 3.i: A Bayesian framework for updating the model for end-stage liver disease score
IF 7.5
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
Abstract
Background & Aims
The model for end-stage liver disease (MELD) score has been central to liver transplant (LT) allocation since 2002, with iterative updates culminating in MELD 3.0. However, given temporal changes and variations in liver disease epidemiology across allocation systems that utilize MELD, continuous refinements are essential to ensure its optimal performance across diverse patient populations and transplant frameworks.
Methods
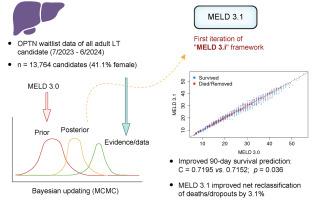
This retrospective cohort study included all US adult LT candidates listed between July 13, 2023 to June 30, 2024. Candidates from the first two-thirds of listing dates formed the training set, while the last third comprised the validation set. We applied a Bayesian proportional hazards model, using MELD 3.0 as informative priors to generate posterior coefficient distributions. The resulting model, MELD 3.1, represents the first iteration within the MELD 3.i framework. Model performance was assessed using concordance (C-) statistics, and reclassification analyses evaluated patient redistribution and mortality risk across MELD tiers.
Results
The cohort included 13,764 candidates (41.1% female). MELD 3.1 assigned a higher coefficient for female sex and a lower coefficient for creatinine, and showed improved C-statistics for 90-day waitlist mortality in the validation set (0.7195 vs. 0.7152 for MELD 3.0, p = 0.036). MELD 3.1 led to a net 3.1% up-categorization of patients who died or dropped out while on the waitlist, with the net gain entirely accounted for by female candidates. MELD 3.1 also showed net gains across age groups and liver disease etiologies.
Conclusion
Our findings provide proof-of-concept for the MELD updating framework (MELD 3.i) as a sustainable and adaptive approach for periodically refining MELD using contemporary data and Bayesian methods. This iterative process enhances predictive accuracy, ensuring MELD remains responsive to evolving demographics and clinical practices in the US and other allocation systems.
Impact and implications
We present MELD 3.i, a Bayesian framework for ongoing refinement of the MELD score, with MELD 3.1 as its first iteration. The findings demonstrate improved predictive accuracy for 90-day waitlist mortality compared to the original MELD 3.0, particularly for women. These results are important for clinicians, transplant centers, and policymakers aiming to optimize organ allocation while addressing persistent sex disparities. By enabling adaptive refinements within an existing model structure, this approach has the potential to offer a practical method to align liver transplant prioritization with evolving patient demographics and varying practices across nations and regions.
融合3。i:更新终末期肝病评分模型的贝叶斯框架
自2002年以来,终末期肝病(MELD)评分模型一直是肝移植(LT)分配的核心,随着MELD 3.0的不断更新,该模型达到了顶峰。然而,考虑到使用MELD的分配系统中肝脏疾病流行病学的时间变化和差异,持续改进是确保其在不同患者群体和移植框架中的最佳性能所必需的。方法本回顾性队列研究纳入了2023年7月13日至2024年6月30日期间列出的所有美国成人LT候选人。列表日期的前三分之二的候选对象组成训练集,而最后三分之一的候选对象组成验证集。我们采用贝叶斯比例风险模型,使用MELD 3.0作为信息先验来生成后验系数分布。得到的模型,MELD 3.1,代表了MELD 3中的第一次迭代。我的框架。使用一致性(C-)统计来评估模型的性能,再分类分析评估了MELD各层级的患者再分配和死亡风险。结果入选患者13764人,其中女性41.1%。MELD 3.1赋予女性更高的系数和更低的肌酐系数,并显示验证集中90天等待名单死亡率的c统计数据有所改善(0.7195 vs. MELD 3.0的0.7152,p = 0.036)。MELD 3.1导致在等待名单上死亡或退出的患者的分类净增3.1%,净增完全由女性候选人占。MELD 3.1也显示出各年龄组和肝病病因的净收益。结论我们的研究结果为MELD更新框架(MELD 3)提供了概念验证。i)作为使用当代数据和贝叶斯方法定期改进MELD的可持续和适应性方法。这种迭代过程提高了预测的准确性,确保MELD保持对美国和其他分配系统不断变化的人口统计和临床实践的响应。影响和启示我们提出MELD 3。i,用于持续改进MELD评分的贝叶斯框架,MELD 3.1是其第一次迭代。研究结果表明,与最初的MELD 3.0相比,对90天等待名单死亡率的预测准确性有所提高,尤其是对女性。这些结果对于临床医生、移植中心和决策者在解决持续存在的性别差异的同时优化器官分配具有重要意义。通过在现有模型结构中进行适应性改进,该方法有可能提供一种实用的方法,使肝移植优先级与不断变化的患者人口统计数据和不同国家和地区的不同实践保持一致。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

JHEP Reports
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
12.40
自引率
2.40%
发文量
161
审稿时长
36 days
期刊介绍:
JHEP Reports is an open access journal that is affiliated with the European Association for the Study of the Liver (EASL). It serves as a companion journal to the highly respected Journal of Hepatology.
The primary objective of JHEP Reports is to publish original papers and reviews that contribute to the advancement of knowledge in the field of liver diseases. The journal covers a wide range of topics, including basic, translational, and clinical research. It also focuses on global issues in hepatology, with particular emphasis on areas such as clinical trials, novel diagnostics, precision medicine and therapeutics, cancer research, cellular and molecular studies, artificial intelligence, microbiome research, epidemiology, and cutting-edge technologies.
In summary, JHEP Reports is dedicated to promoting scientific discoveries and innovations in liver diseases through the publication of high-quality research papers and reviews covering various aspects of hepatology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


