Partner status and partner mental health and the risk of postpartum depression
IF 8.7
引用次数: 0
Abstract
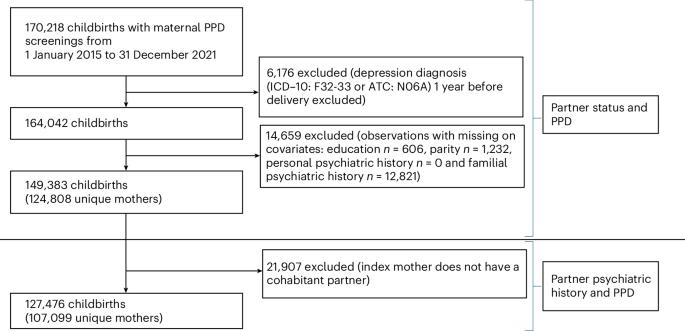
Although the association between partner status and postpartum depression (PPD) is well studied, less is known about how a partner’s psychiatric history affects PPD risk in partnered mothers. Here, using maternal PPD screenings merged with Danish registers from 149,383 childbirths, we examined the influence of partner status and partner mental health on PPD risk. Exposures were partner status and partner psychiatric history, and outcomes were PPD (positive screening) and severe PPD (antidepressants or diagnosis). In total, 14.7% were unpartnered mothers, with a higher risk of PPD (absolute risk (AR) 8.9% versus 7.0%; relative risk (RR) 1.11 (95% confidence interval (CI) 1.05–1.16)) and severe PPD (AR 1.1% versus 0.9%; RR 0.99 (95% CI 0.86–1.14)) compared with partnered mothers. Among partnered mothers, 19.7% had partners with psychiatric history. Recent psychiatric history increased the risk of PPD (AR 8.3%; RR 1.10 (95% CI 1.02–1.18)) and severe PPD (AR 1.5%; RR 1.42 (95% CI 1.18–1.69)), compared with no psychiatric history. We show that unpartnered mothers face a slightly increased PPD risk, while recent partner psychiatric episodes markedly increase risk in partnered mothers. In this study, Zacher Kjeldsen and colleagues examine the role of partner mental health in maternal postpartum depression risk.
伴侣状况、伴侣心理健康和产后抑郁症的风险
尽管伴侣状态与产后抑郁症(PPD)之间的关系已经得到了很好的研究,但对于伴侣的精神病史如何影响有伴侣的母亲患产后抑郁症的风险,人们知之甚少。在这里,我们将149,383例分娩的产妇PPD筛查与丹麦登记册合并,研究了伴侣状态和伴侣心理健康对PPD风险的影响。暴露是伴侣状态和伴侣精神病史,结果是PPD(阳性筛查)和严重PPD(抗抑郁药物或诊断)。总的来说,14.7%是无伴侣的母亲,PPD的风险更高(绝对风险(AR) 8.9%对7.0%;相对危险度(RR) 1.11(95%可信区间(CI) 1.05-1.16))和严重PPD (AR 1.1% vs 0.9%; RR 0.99 (95% CI 0.86-1.14))。在有伴侣的母亲中,19.7%的伴侣有精神病史。与没有精神病史的患者相比,近期精神病史增加了PPD的风险(AR为8.3%;RR为1.10 (95% CI 1.02-1.18))和重度PPD (AR为1.5%;RR为1.42 (95% CI 1.18-1.69))。我们发现,没有伴侣的母亲患产后抑郁症的风险略有增加,而有伴侣的母亲最近的精神疾病发作明显增加了患产后抑郁症的风险。在这项研究中,Zacher Kjeldsen及其同事研究了伴侣心理健康在母亲产后抑郁风险中的作用。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


