Association between urban shrinkage and excess mortality during the COVID-19 pandemic
引用次数: 0
Abstract
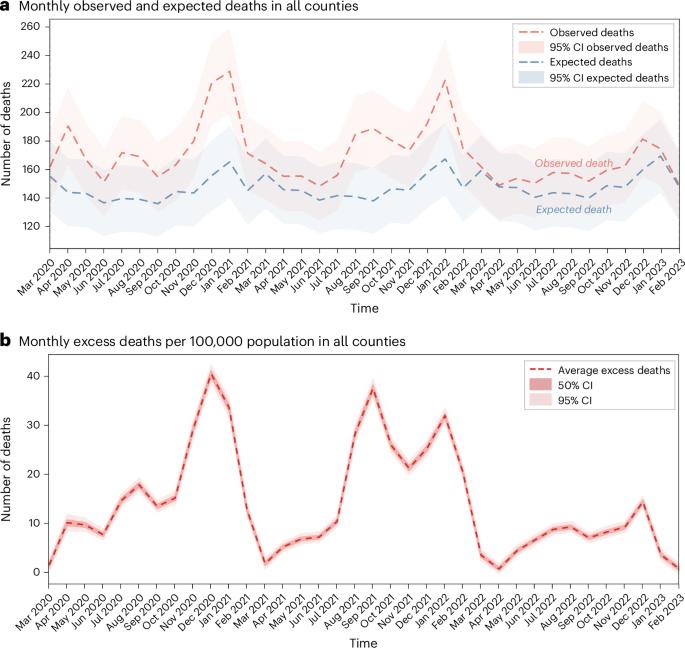
As the COVID-19 pandemic exposed and amplified structural vulnerabilities in cities, understanding how urban shrinkage exacerbates public health risks has become increasingly urgent. This study examines the relationship between urban shrinkage and excess mortality in 1,142 US counties during the COVID-19 pandemic (March 2020–February 2023). Using Kruskal–Wallis tests and mixed-effects models, we analyzed how different patterns and degrees of urban shrinkage influenced monthly excess deaths per 100,000 population and the frequency of mortality peaks. The results indicate that shrinking counties showed 165% higher excess deaths and 142% more mortality peaks than growing counties. Notably, counties experiencing simultaneous declines in both population and gross regional domestic product demonstrated worse outcomes than those with only one dimension of shrinkage. Furthermore, excess deaths increased proportionally with the severity of demographic and economic contraction. Socioeconomic disadvantages prevalent in shrinking counties—including lower income levels, higher proportions of older adults, lower educational attainment and higher unemployment rates—were also associated with elevated excess deaths. These findings underscore the need for place-based public health strategies tailored to address the structural vulnerabilities faced by shrinking and socioeconomically disadvantaged communities. Shrinking US counties faced 165% higher COVID-19 excess mortality than growing areas, exacerbated by combined population and economic decline. Structural vulnerabilities in shrinking regions underscore the need for targeted health interventions addressing socioeconomic disparities.
2019冠状病毒病大流行期间城市萎缩与过高死亡率之间的关系
随着2019冠状病毒病大流行暴露并放大了城市的结构性脆弱性,了解城市收缩如何加剧公共卫生风险变得越来越紧迫。本研究考察了2019冠状病毒病大流行期间(2020年3月至2023年2月)美国1142个县的城市收缩与超额死亡率之间的关系。利用Kruskal-Wallis检验和混合效应模型,我们分析了城市收缩的不同模式和程度如何影响每10万人每月超额死亡率和死亡率峰值的频率。结果表明,萎缩县的超额死亡率比增长县高165%,死亡率峰值比增长县高142%。值得注意的是,人口和地区国内生产总值同时下降的国家,其结果比那些只有一个维度萎缩的国家更糟糕。此外,超额死亡人数随着人口和经济收缩的严重程度成比例地增加。在萎缩的国家中普遍存在的社会经济劣势——包括收入水平较低、老年人比例较高、受教育程度较低和失业率较高——也与过高的死亡率有关。这些调查结果强调,需要制定基于地方的公共卫生战略,以解决日益缩小和社会经济上处于不利地位的社区面临的结构性脆弱性。萎缩的美国县的COVID-19超额死亡率比增长地区高165%,人口和经济的综合下降加剧了这一情况。缩小区域的结构性脆弱性突出表明,需要采取有针对性的卫生干预措施,解决社会经济差距问题。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


