Relationship between interleukin-6, coronary artery calcium and risk of heart failure: Insights from MESA
IF 5.9
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
This study investigated the joint association of interleukin-6 (IL-6) and coronary artery calcium (CAC) with the risk of heart failure (HF).
Methods and Results
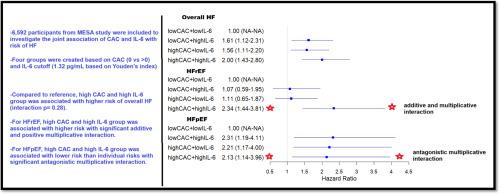
Among 6592 participants in the Multi-Ethnic Study of Atherosclerosis (MESA), individuals were categorized into four groups based on CAC (0 vs >0) and IL-6 (cutoff 1.32 pg/mL via Youden’s index): low CAC/low IL-6 (reference), low CAC/high IL-6, high CAC/low IL-6, and high CAC/high IL-6. Multivariable Cox models were used to assess the risk of total heart failure (HF), HF with reduced ejection fraction (HFrEF), and HF with preserved ejection fraction (HFpEF). Compared to the reference group, the hazard ratios (HRs) for total HF were 1.61 (95 % CI, 1.12–2.31) for high IL-6, 1.56 (95 % CI, 1.11–2.20) for high CAC, and 2.00 (95 % CI, 1.43–2.80) when both were elevated (multiplicative interaction p = 0.28). For HFrEF, the risk was significantly higher only when both markers were elevated: HR 2.34 (95 % CI, 1.44–3.81), compared to isolated CAC (1.11; 95 % CI, 0.65–1.87) or IL-6 (1.07; 95 % CI, 0.59–1.95) (multiplicative and additive interaction p = 0.05 and 0.008, respectively). Conversely, for HFpEF, the combined elevation of IL-6 and CAC was associated with a lower risk than either marker alone: HRs 2.13, 2.31, and 2.21, respectively (antagonistic multiplicative interaction, p = 0.02).
Conclusions
Combined elevation of IL-6 and CAC was associated with increased HFrEF risk, with significant additive and multiplicative interactions. For HFpEF, combined elevation conferred less risk than either alone. Inflammation modifies the CAC![]() HFrEF relationship and merits further study.
HFrEF relationship and merits further study.
白细胞介素-6、冠状动脉钙与心力衰竭风险的关系:来自MESA的见解
本研究探讨了白细胞介素-6 (IL-6)和冠状动脉钙(CAC)与心力衰竭(HF)风险的联合关系。方法和结果在多民族动脉粥样硬化研究(MESA)的6592名参与者中,根据CAC (0 vs >0)和IL-6(通过约登指数截止1.32 pg/mL)将个体分为四组:低CAC/低IL-6(参考),低CAC/高IL-6,高CAC/低IL-6和高CAC/高IL-6。采用多变量Cox模型评估全心力衰竭(HF)、HF伴射血分数降低(HFrEF)和HF伴射血分数保留(HFpEF)的风险。与对照组相比,高IL-6组总HF的风险比(hr)为1.61 (95% CI, 1.12-2.31),高CAC组的风险比为1.56 (95% CI, 1.11-2.20),两者均升高时的风险比(hr)为2.00 (95% CI, 1.43-2.80)(乘积相互作用p = 0.28)。对于HFrEF,只有当两种标记物都升高时,风险才会显著增加:HR为2.34 (95% CI, 1.44-3.81),与分离的CAC (1.11, 95% CI, 0.65-1.87)或IL-6 (1.07, 95% CI, 0.59-1.95)相比(乘法和加性相互作用p分别= 0.05和0.008)。相反,对于HFpEF, IL-6和CAC联合升高的风险低于单独使用任何一种标志物:hr分别为2.13、2.31和2.21(拮抗乘法相互作用,p = 0.02)。结论IL-6和CAC联合升高与HFrEF风险增加相关,存在显著的叠加性和倍增性相互作用。对于HFpEF,联合抬高比单独抬高的风险更小。炎症改变了CACHFrEF的关系,值得进一步研究。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

American journal of preventive cardiology
Cardiology and Cardiovascular Medicine
CiteScore
6.60
自引率
0.00%
发文量
0
审稿时长
76 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


