Altered neurovascular-cerebrospinal fluid synergy in chronic insomnia disorder
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
Abstract
Background
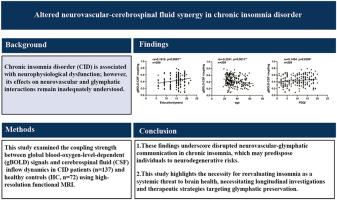
Chronic insomnia disorder (CID) is associated with neurophysiological dysfunction; however, its effects on neurovascular and glymphatic interactions remain inadequately understood.
Methods
This study examined the coupling strength between global blood-oxygen-level-dependent (gBOLD) signals and cerebrospinal fluid (CSF) inflow dynamics in CID patients (n = 137) and healthy controls (HC, n = 72) using resting state functional magnetic resonance imaging.
Results
Results demonstrated significantly diminished gBOLD-CSF coupling in CID patients compared to HC. Across all participants, coupling strength exhibited a negative correlation with age and a positive correlation with educational attainment. Counterintuitively, higher Pittsburgh Sleep Quality Index (PSQI) scores, indicative of poorer sleep quality, were associated with stronger BOLD-CSF coupling, potentially reflecting compensatory mechanisms during infrequent deep sleep episodes.
Conclusion
These findings underscore disrupted neurovascular-glymphatic communication in chronic insomnia, which may predispose individuals to neurodegenerative risks. This study highlights the necessity for reevaluating insomnia as a systemic threat to brain health, necessitating longitudinal investigations and therapeutic strategies targeting glymphatic preservation.
慢性失眠症中神经血管-脑脊液协同作用的改变
背景:慢性失眠障碍(CID)与神经生理功能障碍有关;然而,其对神经血管和淋巴相互作用的影响仍不充分了解。方法采用静息状态功能磁共振成像技术检测CID患者(n = 137)和健康对照(n = 72)的全血氧水平依赖(gBOLD)信号与脑脊液(CSF)流入动力学之间的耦合强度。结果显示,与HC相比,CID患者的gBOLD-CSF偶联显著降低。在所有参与者中,耦合强度与年龄呈负相关,与受教育程度呈正相关。与直觉相反的是,较高的匹兹堡睡眠质量指数(PSQI)分数表明较差的睡眠质量,与较强的BOLD-CSF耦合相关,可能反映了在不频繁的深度睡眠发作期间的代偿机制。结论这些发现强调了慢性失眠中神经血管-淋巴通讯的中断,这可能使个体易患神经退行性风险。这项研究强调了重新评估失眠对大脑健康的系统性威胁的必要性,需要纵向调查和针对淋巴细胞保存的治疗策略。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


