Independent association between hourly apnea-hypopnea duration and prevalence of diabetes in male adults
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
Abstract
Objective
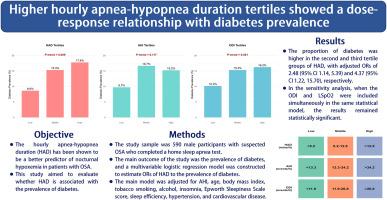
Although the apnea-hypopnea index (AHI) is currently used as a diagnostic indicator to assess the severity of obstructive sleep apnea (OSA), the AHI alone cannot adequately identify the risk of diabetes mellitus. On the other hand, the hourly apnea-hypopnea duration (HAD) has been shown to be a better predictor of nocturnal hypoxemia in patients with OSA. This study aimed to evaluate whether HAD is associated with the prevalence of diabetes.
Methods
The study sample was 590 male participants with suspected OSA who completed a home sleep apnea test. The main outcome of the study was the prevalence of diabetes, and a multivariable logistic regression model was constructed to estimate the odds ratio (ORs) of HAD to the prevalence of diabetes. The main model was adjusted for AHI, age, body mass index, tobacco smoking, alcohol, insomnia, Epworth Sleepiness Scale score, sleep efficiency, hypertension, and cardiovascular disease.
Results
The prevalence of diabetes was 13.90 % in the selected population (quartile age 48.00–68.00 years). The proportion of diabetes was higher in the second and third tertile groups of HAD, with adjusted ORs of 2.48 (95 % CI 1.14, 5.39) and 4.37 (95 % CI 1.22, 15.70), respectively. In the sensitivity analysis, when the oxygen desaturation index (ODI) and lowest oxygen saturation by pulse oximetry were included simultaneously in the same statistical model, the results remained statistically significant. In the multivariable regression analysis, neither AHI nor ODI showed a significant association with the prevalence of diabetes (P > 0.05).
Conclusion
After adjusting for multiple potential confounders, higher HAD tertiles were associated with a higher prevalence of diabetes. In the clinical assessment of OSA-related adverse health outcomes, the HAD deserves more consideration.
男性成人每小时呼吸暂停-低通气持续时间与糖尿病患病率之间的独立关联。
目的:虽然目前使用呼吸暂停低通气指数(AHI)作为评估阻塞性睡眠呼吸暂停(OSA)严重程度的诊断指标,但仅用AHI不能充分识别糖尿病的风险。另一方面,每小时呼吸暂停低通气持续时间(HAD)已被证明是OSA患者夜间低氧血症的更好预测指标。本研究旨在评估HAD是否与糖尿病患病率相关。方法:研究样本为590名疑似阻塞性睡眠呼吸暂停的男性参与者,他们完成了家庭睡眠呼吸暂停测试。本研究的主要结局为糖尿病患病率,并构建多变量logistic回归模型来估计HAD与糖尿病患病率的比值比(ORs)。对主要模型进行了AHI、年龄、体重指数、吸烟、饮酒、失眠、Epworth嗜睡量表评分、睡眠效率、高血压、心血管疾病等因素的调整。结果:所选人群(四分位数年龄48.00 ~ 68.00岁)糖尿病患病率为13.90%。糖尿病的比例在HAD的第二组和第三组较高,调整后的or分别为2.48 (95% CI 1.14, 5.39)和4.37 (95% CI 1.22, 15.70)。在敏感性分析中,将氧去饱和指数(ODI)和脉搏血氧仪最低血氧饱和度同时纳入同一统计模型,结果仍具有统计学意义。在多变量回归分析中,AHI和ODI与糖尿病患病率均无显著相关性(P < 0.05)。结论:在对多个潜在混杂因素进行校正后,较高的HAD分位数与较高的糖尿病患病率相关。在临床评估osa相关的不良健康结果时,HAD值得更多的考虑。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


