Cardiac resynchronization therapy in chronic Chagas cardiomyopathy: A systematic review and single-arm meta-analysis
IF 2.9
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
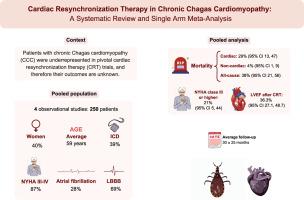
Cardiac resynchronization therapy (CRT) is a well-established therapy for patients with heart failure. However, patients with chronic Chagas cardiomyopathy (CCC) were underrepresented in pivotal CRT trials.
Objective
This systematic review and meta-analysis aim to quantitatively describe the outcomes of CRT in patients with CCC.
Methods
We systematically searched PubMed, Embase, Cochrane, and LILACS registries for studies evaluating the response to CRT in patients with CCC. We applied no language or date restrictions. We applied an inverse-variance random-effects model for a meta-analysis of proportions.
Results
We included 4 observational cohort studies comprising 250 patients with CCC undergoing CRT. At CRT implantation, the mean age was 59 ± 12 years, 87% of patients (217) were New York Heart Association class III/IV, and the average left ventricular ejection fraction (LVEF) was 27% ± 7%. During a mean follow-up of 30 ± 25 months, the all-cause death rate was 38% (95% confidence interval [CI], 21–56), cardiac death rate was 29% (95% CI, 13–47), and the noncardiac death rate was 4% (95% CI, 1–9). After CRT, the proportion of patients rated New York Heart Association class III/IV was improved to 21% (95% CI, 5–44), with a pooled post-CRT LVEF of 36.3% (95% CI, 27.0–48.0).
Conclusion
In patients with CCC, CRT was associated with improvements in LVEF and symptomatic and functional burden (class III/IV), but overall mortality remained high. Although CRT seems to be beneficial in this population, further research is warranted to better characterize its impact on long-term clinical outcomes.
慢性Chagas心肌病的心脏再同步化治疗:系统回顾和单组荟萃分析
背景:心脏再同步化治疗(CRT)是治疗心力衰竭的一种行之有效的治疗方法。然而,慢性恰加斯心肌病(CCC)患者在关键性CRT试验中的代表性不足。目的本系统综述和荟萃分析旨在定量描述CRT治疗CCC患者的结果。方法我们系统地检索PubMed、Embase、Cochrane和LILACS注册库,以评估CCC患者对CRT的反应。我们没有使用语言或日期限制。我们应用了一个反方差随机效应模型来进行比例的荟萃分析。结果我们纳入了4项观察性队列研究,包括250例接受CRT治疗的CCC患者。植入CRT时,平均年龄59±12岁,87%(217例)患者为纽约心脏协会III/IV级,平均左室射血分数(LVEF)为27%±7%。平均随访30±25个月,全因死亡率为38%(95%可信区间[CI], 21-56),心源性死亡率为29% (95% CI, 13-47),非心源性死亡率为4% (95% CI, 1-9)。CRT后,纽约心脏协会III/IV级患者比例提高至21% (95% CI, 5-44), CRT后LVEF合计为36.3% (95% CI, 27.0-48.0)。结论在CCC患者中,CRT与LVEF的改善以及症状和功能负担(III/IV级)相关,但总体死亡率仍然很高。虽然CRT在这一人群中似乎是有益的,但需要进一步的研究来更好地表征其对长期临床结果的影响。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Heart Rhythm O2
Cardiology and Cardiovascular Medicine
CiteScore
3.30
自引率
0.00%
发文量
0
审稿时长
52 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


