Budd–Chiari Syndrome and Pregnancy—A Review
IF 3.2
Q2 GASTROENTEROLOGY & HEPATOLOGY
Journal of Clinical and Experimental Hepatology
Pub Date : 2025-08-26
DOI:10.1016/j.jceh.2025.103176
引用次数: 0
Abstract
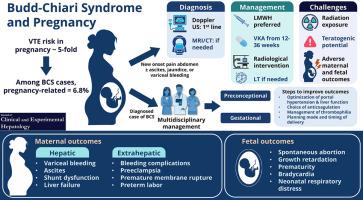
Pregnancy is a hypercoagulable state, increasing the risk of venous thrombosis, including Budd–Chiari syndrome (BCS). Historically, pregnancy was contraindicated in BCS due to risks like hepatic dysfunction, thrombosis, bleeding, and poor fetal outcomes. However, better diagnostic modalities, greater awareness, and treatment advances, such as anticoagulant therapy, endovascular interventions like hepatic vein angioplasty with or without stenting, transjugular intrahepatic portosystemic shunt (TIPS), and liver transplantation (LT), have enabled more favorable outcomes. When BCS presents during pregnancy, diagnosis can be challenging, often mimicking other pregnancy-related liver conditions. Doppler ultrasonography is the preferred diagnostic tool during pregnancy, with cross-sectional imaging reserved for doubtful cases and planning intervention. Anticoagulation is the cornerstone of medical therapy for BCS diagnosed in pregnancy, preventing thrombus progression. Radiological interventions like hepatic vein stenting and TIPS are options, particularly for those not responding to medical therapy, though radiation exposure is a consideration, and dose-reduction strategies are employed. LT is a consideration for acute liver failure, with good maternal but suboptimal fetal outcomes. For women with pre-existing BCS planning pregnancy, preconceptional management is crucial. This includes individualized risk assessment, optimizing BCS treatment, and screening for thrombophilia. Delayed diagnosis, advanced age, and progression to cirrhosis may all contribute to infertility in BCS, which need to be considered. However, successful BCS treatment can improve fertility and pregnancy outcomes. Antenatal, perinatal, and postpartum management requires careful monitoring of liver function, portal hypertension, anticoagulation, and fetal well-being, aimed at preventing complications like hemorrhage. Proactive management significantly improves the prognosis for pregnancy in BCS patients.
Budd-Chiari综合征与妊娠a综述
妊娠是高凝状态,增加静脉血栓形成的风险,包括Budd-Chiari综合征(BCS)。从历史上看,由于肝功能障碍、血栓形成、出血和胎儿结局不良等风险,妊娠是BCS的禁忌症。然而,更好的诊断方式,更大的认识和治疗进展,如抗凝治疗,血管内干预,如肝静脉成形术伴或不伴支架植入,经颈静脉肝内门静脉分流术(TIPS)和肝移植(LT),已经实现了更有利的结果。当BCS在怀孕期间出现时,诊断可能具有挑战性,通常会模仿其他与妊娠相关的肝脏疾病。多普勒超声是妊娠期间首选的诊断工具,对可疑病例和计划干预保留横断面成像。抗凝治疗是妊娠期诊断为BCS的药物治疗的基础,可防止血栓进展。像肝静脉支架置入和TIPS这样的放射干预是可选择的,特别是对于那些对药物治疗没有反应的人,尽管辐射暴露是一个考虑因素,并采用了剂量减少策略。肝移植是急性肝功能衰竭的一种考虑,母体预后良好,但胎儿预后欠佳。对于已有BCS的妇女计划怀孕,孕前管理是至关重要的。这包括个体化风险评估、优化BCS治疗和血栓性疾病筛查。延迟诊断、高龄和进展为肝硬化都可能导致BCS患者不孕,这些都需要考虑。然而,成功的BCS治疗可以提高生育能力和妊娠结局。产前、围产期和产后管理需要仔细监测肝功能、门脉高压、抗凝和胎儿健康,以预防出血等并发症。积极治疗可显著改善BCS患者妊娠预后。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Clinical and Experimental Hepatology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
4.90
自引率
16.70%
发文量
537
审稿时长
64 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


