Markedly Low Prevalence of Fatty Liver Despite Obesity in Prader–Willi Syndrome: A Search for Protective Genetic Markers
IF 3.2
Q2 GASTROENTEROLOGY & HEPATOLOGY
Journal of Clinical and Experimental Hepatology
Pub Date : 2025-08-22
DOI:10.1016/j.jceh.2025.103155
引用次数: 0
Abstract
Introduction and objectives
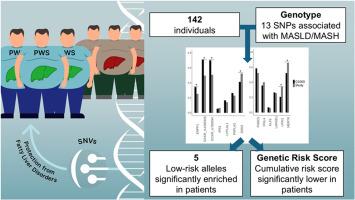
Metabolic dysfunction-associated steatotic liver disease (MASLD) is the most common liver disease across all age groups and is associated with significant morbidity and mortality. The pathogenesis of the disease is not fully understood, but genetic factors appear to play a major role in the development of MASLD. Prader–Willi syndrome (PWS) is a neurogenetic, multisystem disorder characterized primarily by hyperphagia, leading to uncontrolled eating and severe obesity. Despite the high prevalence of severe obesity in PWS, MASLD is relatively rare. The aim of this study was to assess whether single-nucleotide variants (SNVs) known to be associated with MASLD may play a role in the development of MASLD in individuals with PWS.
Patients and methods
Using targeted amplicon-next-generation sequencing, we studied DNA from 142 individuals (69 females), with a median age of 17.5 years, with genetically confirmed PWS, and genotyped 13 SNVs that were previously associated with a high risk for MASLD.
Results
Body mass index (BMI) z-score was 2.1 9IQR: 1.42, 2.490, and the median alanine aminotransferase and aspartate aminotransferase were 18 (IQR: 14, 25) units/L and 24 (IQR: 19, 32) units/L, respectively. Five of the 13 SNVs showed significantly lower frequencies of the risk allele in our cohort compared to frequencies reported in the general population. The cumulative risk score for all 13 SNVs was significantly lower in our cohort of PWS patients compared to the healthy population (FDR-adjusted P-value, 1.85 × 10−5).
Conclusions
We identified genetic factors that may protect patients with PWS from developing MASLD. These findings may contribute to understanding the pathogenesis of MASLD in individuals with nonsyndromic obesity.
在Prader-Willi综合征中,尽管肥胖,但脂肪肝的患病率明显较低:对保护性遗传标记的研究
简介和目的代谢功能障碍相关脂肪变性肝病(MASLD)是所有年龄组中最常见的肝脏疾病,与显著的发病率和死亡率相关。该疾病的发病机制尚不完全清楚,但遗传因素似乎在MASLD的发展中起主要作用。普瑞德-威利综合征(PWS)是一种神经遗传性多系统疾病,主要表现为暴饮暴食,导致饮食不受控制和严重肥胖。尽管PWS中严重肥胖的患病率很高,但MASLD相对罕见。本研究的目的是评估已知与MASLD相关的单核苷酸变异(snv)是否可能在PWS患者的MASLD发展中发挥作用。研究人员利用新一代靶向扩增子测序技术,研究了142名个体(69名女性)的DNA,这些个体的中位年龄为17.5岁,遗传上证实患有PWS,并对13个先前与MASLD高风险相关的snv进行了基因分型。结果体重指数(BMI) z-score为2.1 9IQR: 1.42、2.490,中位丙氨酸转氨酶和天冬氨酸转氨酶分别为18 (IQR: 14、25)和24 (IQR: 19、32)单位/L。13个snv中有5个显示我们队列中风险等位基因的频率明显低于一般人群中报告的频率。与健康人群相比,我们的PWS患者队列中所有13个snv的累积风险评分显著降低(经fdr校正的p值为1.85 × 10−5)。结论我们发现了可能保护PWS患者不发生MASLD的遗传因素。这些发现可能有助于理解非综合征性肥胖患者MASLD的发病机制。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Clinical and Experimental Hepatology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
4.90
自引率
16.70%
发文量
537
审稿时长
64 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


