Ischemia-modified albumin and cardiovascular risk in obstructive sleep apnea and acute coronary syndrome. Long term follow-up after treatment from the ISAACC study
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
Abstract
Introduction
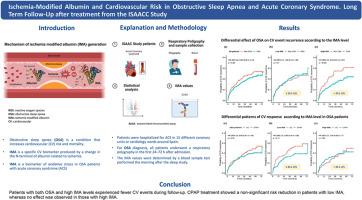
In the context of the prevailing interest in biomarkers that can assess cardiovascular (CV) risk in obstructive sleep apnea (OSA), ischemia-modified albumin (IMA) is proposed as a potential risk predictor.
Objectives
To evaluate whether IMA levels predict recurrent CV events in patients with acute coronary syndrome (ACS) and OSA, and whether continuous positive airway pressure (CPAP) treatment modifies this risk.
Methods
This post hoc analysis is based on data from the ISAACC study, including 1.011 non-sleepy patients with an ACS. During hospitalization for ACS, a sleep study was conducted and blood samples for IMA determination were obtained. Patients were categorized by their apnea–hypopnea index (AHI) in non-OSA (AHI <15 events/h) or OSA group (AHI ≥15 events/h). “Low” or “high” IMA levels were established based on the median value (⩽ 34.1 U/L or > 34.1 U/L, respectively). The OSA group was randomized to either CPAP or usual care. The recurrence of CV events was evaluated over a 36-months follow-up.
Results
Adjusted cox regression models showed that the OSA group with high IMA level had a significantly reduced risk for CV event recurrence compared with the non-OSA group (HR [95 % CI] 0.59 [0.38–0.93], p = 0.024). In the OSA group with high IMA level, CPAP treatment did not significantly reduce CV recurrence.
Conclusions
OSA was associated with higher IMA levels in patients with ACS. Interestingly, patients with both OSA and high IMA experienced fewer CVEs during follow-up. CPAP treatment demonstrated a non-significant risk reduction in patients with low IMA, whereas no effect was noted in those with high IMA.
缺血修饰白蛋白与阻塞性睡眠呼吸暂停和急性冠状动脉综合征的心血管风险。ISAACC研究治疗后的长期随访
在对可评估阻塞性睡眠呼吸暂停(OSA)患者心血管(CV)风险的生物标志物普遍感兴趣的背景下,缺血修饰白蛋白(IMA)被提出作为一种潜在的风险预测因子。目的评估IMA水平是否能预测急性冠脉综合征(ACS)和OSA患者的心血管事件复发,以及持续气道正压通气(CPAP)治疗是否能改变这一风险。方法本事后分析基于ISAACC研究的数据,包括1.011例非困倦ACS患者。在ACS住院期间,进行了睡眠研究,并获得了血液样本用于IMA测定。根据患者的呼吸暂停低通气指数(AHI)分为非OSA组(AHI≤15事件/小时)和OSA组(AHI≥15事件/小时)。“低”或“高”IMA水平是根据中位数(分别为≤34.1 U/L或≤34.1 U/L)确定的。OSA组随机分为CPAP组和常规治疗组。在36个月的随访中评估CV事件的复发情况。结果经校正的cox回归模型显示,与非OSA组相比,IMA水平高的OSA组CV事件复发风险显著降低(HR [95% CI] 0.59 [0.38-0.93], p = 0.024)。在IMA水平较高的OSA组中,CPAP治疗没有显著降低CV复发率。结论sosa与ACS患者较高的IMA水平相关。有趣的是,OSA和高IMA患者在随访期间的cve经历较少。CPAP治疗显示低IMA患者的风险降低不显著,而高IMA患者则没有效果。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


