Dubin–Johnson Syndrome: An Eight-Year Retrospective Clinicopathological Review from a North Indian Tertiary Center
IF 3.2
Q2 GASTROENTEROLOGY & HEPATOLOGY
Journal of Clinical and Experimental Hepatology
Pub Date : 2025-08-22
DOI:10.1016/j.jceh.2025.103159
引用次数: 0
Abstract
Background and aims
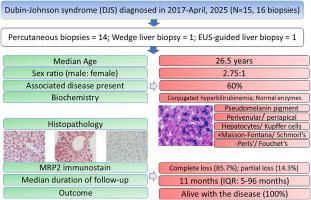
Dubin–Johnson syndrome (DJS) is an uncommon disease with a characteristic clinical and biochemical profile, rarely requiring diagnostic liver biopsy. Indian data on the clinicopathological spectrum of DJS are scant. The study is aimed at the analysis of the clinical context for liver biopsy, histological spectrum, utility of special stains, and multidrug resistance-associated protein 2 (MRP2) immunohistochemistry in DJS.
Materials and methods
The clinical presentation, hematological, and biochemical parameters of all biopsy-proven cases of DJS in the last eight years (N = 15, 16 biopsies) were gleaned from the archives. All biopsies were stained with routine hematoxylin and eosin stain, various special stains, MRP2, bile salt export pump, and CK7 immunostains.
Results
The median age of presentation of DJS was 26.5 years (interquartile range [IQR]: 19–60.5 years). Nine of 15 patients (60%) had an additional liver disorder (chronic viral hepatitis, non-cirrhotic portal fibrosis, cirrhosis, etc). One-third of the cases were diagnosed on histology alone (clinically unsuspected). All cases showed conjugated hyperbilirubinemia (median total bilirubin: 5.1 mg/dL, IQR: 4.3–8.1 mg/dL) with normal liver enzymes and hemogram. All biopsies showed centrilobular-dominant deposition of pseudomelanin pigment in the hepatocytes and Kupffer cells. MRP2 immunostain showed complete loss of (85.7%)/partial canalicular (14.3%) expression.
Conclusion
The clinical features of DJS are often obscured/altered by a coexistent liver disease necessitating liver biopsy. Histological documentation of the pigment by a panel of special stains is required for diagnosis. Loss of canalicular MRP2 expression complements special stains when pigment is scant and should be considered in diagnostically challenging biopsies.
杜宾-约翰逊综合征:来自北印度三级中心的八年回顾性临床病理回顾
背景和目的杜宾-约翰逊综合征(DJS)是一种罕见的疾病,具有独特的临床和生化特征,很少需要诊断性肝活检。印度关于dj临床病理谱的数据很少。本研究旨在分析DJS患者肝活检的临床背景、组织学谱、特殊染色的应用以及多药耐药相关蛋白2 (MRP2)免疫组织化学。材料与方法收集近8年来所有经活检证实的DJS病例(15例,16例)的临床表现、血液学及生化指标。所有活检组织均行常规苏木精、伊红染色、各种特殊染色、MRP2、胆盐输出泵、CK7免疫染色。结果发病年龄中位数为26.5岁(四分位数间距[IQR]: 19 ~ 60.5岁)。15例患者中有9例(60%)伴有其他肝脏疾病(慢性病毒性肝炎、非肝硬化门脉纤维化、肝硬化等)。三分之一的病例仅凭组织学诊断(临床未怀疑)。所有病例均表现为偶联性高胆红素血症(总胆红素中位数:5.1 mg/dL, IQR: 4.3-8.1 mg/dL),肝酶和血象正常。所有活组织检查均显示肝细胞和库普弗细胞中以小叶中心为主的假黑色素沉积。MRP2免疫染色显示完全缺失(85.7%)/部分小管表达(14.3%)。结论dj的临床特征常因并发肝脏疾病而模糊或改变,需要进行肝脏活检。诊断时需要用一组特殊染色剂对色素进行组织学记录。当色素缺乏时,小管MRP2表达的缺失补充了特殊的染色,在诊断上具有挑战性的活检中应予以考虑。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Clinical and Experimental Hepatology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
4.90
自引率
16.70%
发文量
537
审稿时长
64 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


