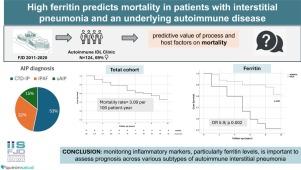
High Ferritin Predicts Mortality in Patients With Interstitial Pneumonia and an Underlying Autoimmune Disease
Q4 Medicine
引用次数: 0
Abstract
Purpose
To identify early predictive markers in patients with chronic interstitial pneumonia (IP) associated with an underlying autoimmune disease (AIP), aiming to facilitate personalized follow-up and treatment.
Methods
We assessed the predictive value of process and host factors on mortality in a cohort of 124 patients (86 women) with autoimmune interstitial pneumonia (AIP). This cohort comprised 66 cases of connective tissue disease-associated interstitial pneumonia (CTD-IP), 40 patients with interstitial pneumonia with autoimmune features (IPAF), and 18 patients with undifferentiated autoimmune IP. All patients had a minimum follow-up of 2 years or a fatal outcome. We included demographics, clinical diagnostic subgroups, specific antibodies, morphological patterns, and relevant laboratory tests in our analysis. For the bivariate analysis, we employed Student's t-test, Fisher's exact test, and survival techniques. Prediction models for death risk were developed using logistic regression.
Results
During the follow-up period, there were 29 deaths, resulting in an incidence rate of 3.09 per 100 patient-year. Factors associated with an increased risk of death included older age at diagnosis, cardio-respiratory comorbidities, and a simultaneous onset of intersticial pneumonia and systemic manifestations. In contrast, clinical diagnosis and radiographic patterns did not show a significant association with mortality risk. Additionally, elevated levels of lactate dehydrogenase, sedimentation rate, C-reactive protein, and ferritin were significantly linked to fatal outcomes. Among these, ferritin emerged as the most potent predictor in the multivariate model, with an odds ratio of 5.9 (p = 0.002).
Conclusion
Our data emphasize the importance of monitoring inflammatory markers, particularly ferritin levels, to assess prognosis across various subtypes of autoimmune intersticial pneumonia.
高铁蛋白可预测间质性肺炎和潜在自身免疫性疾病患者的死亡率
目的探讨慢性间质性肺炎(IP)合并潜在自身免疫性疾病(AIP)患者的早期预测指标,为个性化随访和治疗提供依据。方法对124例自身免疫性间质性肺炎(AIP)患者(86例女性)的过程和宿主因素对死亡率的预测价值进行评估。该队列包括66例结缔组织病相关间质性肺炎(CTD-IP), 40例具有自身免疫性特征的间质性肺炎(IPAF)和18例未分化的自身免疫性IP患者。所有患者至少随访2年或死亡。我们的分析包括人口统计学、临床诊断亚组、特异性抗体、形态模式和相关的实验室测试。对于双变量分析,我们采用了学生t检验、Fisher精确检验和生存技术。采用logistic回归建立死亡风险预测模型。结果随访期间死亡29例,发病率为3.09 / 100患者年。与死亡风险增加相关的因素包括诊断时年龄较大、心肺合并症、间质性肺炎和全身性表现同时发病。相反,临床诊断和放射学模式没有显示出与死亡风险的显著关联。此外,乳酸脱氢酶、沉降率、c反应蛋白和铁蛋白水平升高与死亡结果显著相关。其中,铁蛋白在多变量模型中成为最有效的预测因子,比值比为5.9 (p = 0.002)。结论:我们的数据强调了监测炎症标志物,特别是铁蛋白水平对评估自身免疫性间质性肺炎不同亚型预后的重要性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Open Respiratory Archives
Medicine-Pulmonary and Respiratory Medicine
CiteScore
1.10
自引率
0.00%
发文量
58
审稿时长
51 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


