Outcomes of Iatrogenic Atrial Septal Defect Closure After Transseptal Transcatheter Mitral Valve Replacement in the Mitral Implantation of Transcatheter Valves (MITRAL) Trial
IF 2.8
Q3 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
The long-term hemodynamic consequences of iatrogenic atrial septum defect (iASD) after transseptal (TS) transcatheter mitral valve replacement (TMVR) are unknown. The objective of this study was to compare the clinical outcomes of patients who underwent iASD closure after TS TMVR in the MITRAL (Mitral Implantation of TRAnscatheter vaLves) trial.
Methods
The MITRAL trial enrolled high-surgical-risk patients with severe mitral annular calcification treated with valve-in-mitral annular calcification (ViMAC), failed surgical repair with annuloplasty ring treated with mitral valve-in-ring (MViR), or failed surgical mitral bioprosthesis treated with mitral valve-in-valve (MViV).
Results
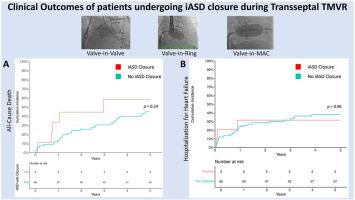
Ninety-one patients were prospectively enrolled between February 2015 and December 2017, at 13 US sites (MViV = 30, MViR = 30, ViMAC = 31). Seventy-five of them were treated with TS access (MViV = 30, MViR = 30, and ViMAC = 15), of which 16 patients underwent iASD closure during or after the index procedure (MViV = 3, MViR = 7, ViMAC = 6). Closure of the iASDs was left to the operator's discretion, and the reason in most patients was the presence of large left-to-right shunt. Patients who underwent closure of iASD were a sicker population at baseline with more severe symptoms (87.5% with New York Heart Association functional class III-IV, compared to 81.4% in non-iASD closure group, p = 0.02), higher rate of recent heart failure hospitalization (68.8% vs. 30.5%; p = 0.01) and lower 6-minute walk test distance (110 m vs. 214 m; p = 0.002). These patients also had longer length of stay after TMVR compared with patients who did not undergo iASD closure (8 vs. 4 days, p < 0.001). Despite these differences at baseline and requiring longer hospital stays, there was no significant difference in mortality, New York Heart Association class, 6-minute walk test distance, or heart failure hospitalization at 5 years.
Conclusions
Patients who underwent iASD closure were more symptomatic at baseline, had decreased functional exercise capacity and required longer length of stay after TMVR. Despite these differences at baseline, 5-year outcomes were similar between groups.
经导管二尖瓣置换术后医源性房间隔缺损关闭的结果
经房间隔(TS)经导管二尖瓣置换术(TMVR)后医源性房间隔缺损(iASD)的长期血流动力学后果尚不清楚。本研究的目的是比较经导管二尖瓣植入(TRAnscatheter vaLves,二尖瓣植入)试验中TS TMVR后行iiasd关闭的患者的临床结果。方法:二尖瓣试验纳入手术高危患者,采用二尖瓣环钙化(ViMAC)治疗严重二尖瓣环钙化(ViMAC),二尖瓣环成形术(MViR)治疗手术修复失败,或二尖瓣环(MViV)治疗手术二尖瓣生物假体失败。结果2015年2月至2017年12月期间,在美国13个地点(MViV = 30, MViR = 30, ViMAC = 31)前瞻性纳入了91例患者。其中75例患者采用TS通路治疗(MViV = 30, MViR = 30, ViMAC = 15),其中16例患者在索引手术期间或之后进行了iASD闭合(MViV = 3, MViR = 7, ViMAC = 6)。ids的关闭留给了操作者的自由裁量权,大多数患者的原因是存在较大的从左到右分流。接受iASD关闭的患者在基线时病情较重,症状更严重(87.5%为纽约心脏协会功能等级III-IV,而非iASD关闭组为81.4%,p = 0.02),近期心力衰竭住院率较高(68.8%对30.5%,p = 0.01), 6分钟步行测试距离较短(110米对214米,p = 0.002)。这些患者在TMVR后的住院时间也比未进行iASD关闭的患者更长(8天对4天,p < 0.001)。尽管在基线和需要更长的住院时间方面存在这些差异,但在死亡率、纽约心脏协会分级、6分钟步行测试距离或5年心力衰竭住院方面没有显著差异。结论闭锁患者在基线时症状更明显,功能运动能力下降,TMVR后需要更长的住院时间。尽管基线存在差异,但两组间的5年结果相似。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Structural Heart
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
1.60
自引率
0.00%
发文量
81
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


