The impacts of blood pressure variability on clinical outcomes in patients with out-of-hospital cardiac arrest
IF 2.4
Q3 CRITICAL CARE MEDICINE
引用次数: 0
Abstract
Background
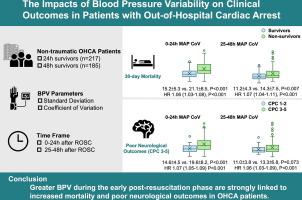
The impact of blood pressure variability (BPV) following out-of-hospital cardiac arrest (OHCA) is not well established. This study aims to investigate the relationship between BPV after the return of spontaneous circulation and clinical outcomes in OHCA patients.
Methods
Non-traumatic OHCA patients were enrolled retrospectively. Continuous intra-arterial blood pressure monitoring was recorded and documented hourly. BPV was assessed using the standard deviation and coefficient of variation within the first 24- and 48-h. The clinical outcomes included 30-day mortality and poor neurological outcomes at discharge, defined as Cerebral Performance Category scale 3–5.
Results
A total of 217 non-traumatic OHCA patients who survived more than 24 h were enrolled. There were 119 deaths within 30 days and 165 poor neurological outcomes at discharge. High BPVs were independently associated with greater risk of 30-day mortality (standard deviation of mean arterial pressure: hazard ratio [HR] = 1.06, 95 % confidence interval [CI] = 1.03–1.10, P < 0.001; coefficient of variation of mean arterial pressure: HR = 1.06, 95 % CI = 1.03–1.08, P < 0.001) and poor neurological outcomes at discharge (standard deviation of mean arterial pressure: HR = 1.08, 95 % CI = 1.05–1.10, P < 0.001; coefficient of variation of mean arterial pressure: HR = 1.07, 95 % CI = 1.05–1.09, P < 0.001). Further analysis on the 185 patients surviving more than 48 h revealed similar findings.
Conclusion
Greater BPV during the early post-resuscitation phase is strongly linked to increased mortality and poor neurological outcomes in OHCA patients.
血压变异性对院外心脏骤停患者临床结局的影响
院外心脏骤停(OHCA)后血压变异性(BPV)的影响尚未得到很好的证实。本研究旨在探讨自然循环恢复后的BPV与OHCA患者临床预后的关系。方法回顾性分析非外伤性OHCA患者。每小时记录和记录连续动脉内血压监测。使用标准偏差和变异系数在前24和48小时内评估BPV。临床结果包括30天死亡率和出院时较差的神经预后,定义为脑功能分类量表3-5。结果共纳入217例存活时间超过24 h的非创伤性OHCA患者。有119人在30天内死亡,165人出院时神经系统预后不良。高bpv与较高的30天死亡风险独立相关(平均动脉压标准差:风险比[HR] = 1.06, 95%可信区间[CI] = 1.03-1.10, P < 0.001;平均动脉压变异系数:HR = 1.06, 95% CI = 1.03-1.08, P < 0.001)和出院时较差的神经预后(平均动脉压标准差:HR = 1.08, 95% CI = 1.05-1.10, P < 0.001;平均动脉压变异系数:HR = 1.07, 95% CI = 1.05-1.09, P < 0.001)。对185例存活超过48小时的患者的进一步分析显示了类似的结果。结论复苏后早期较大的BPV与OHCA患者死亡率增加和神经预后不良密切相关。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Resuscitation plus
Critical Care and Intensive Care Medicine, Emergency Medicine
CiteScore
3.00
自引率
0.00%
发文量
0
审稿时长
52 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


