Prevalence of iron deficiency in patients with mild to moderate bleeding disorders and bleeding disorder of unknown cause
IF 3.4
3区 医学
Q2 HEMATOLOGY
Research and Practice in Thrombosis and Haemostasis
Pub Date : 2025-08-01
DOI:10.1016/j.rpth.2025.102999
引用次数: 0
Abstract
Background
Iron deficiency (ID) and ID anemia (IDA) are often caused by chronic bleeding, especially heavy menstrual bleeding, and thus may occur at a high frequency in patients with mild to moderate bleeding disorders (MBDs).
Objectives
To study the prevalence of iron deficiency in mild to moderate bleeding disorders and bleeding disorder of unknown cause.
Methods
The iron status of patients with MBD from the Vienna Bleeding Biobank, a prospective cohort study, was analyzed and compared with age- and sex-matched healthy controls. ID was defined as ferritin ≤30 μg/L, transferrin saturation <16%, or iron therapy at inclusion. IDA was defined as hemoglobin <12 g/dL in women and <13 g/dL in men diagnosed with ID.
Results
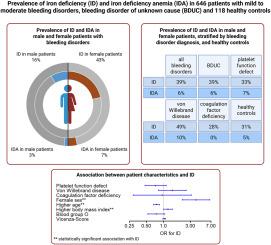
The rates of ID and IDA were comparable between 646 patients with MBD and 118 controls, as 250 patients with MBD (39%) had ID and 40 (6%) had IDA, compared with 37 controls with ID (31%) and 6 with IDA (5%). von Willebrand disease showed a significantly higher rate of ID than controls (49%) before correction for multiple testing, while there was no significant difference between other MBD diagnoses and controls (bleeding disorder of unknown cause: 39%; platelet function disorders: 33%; and coagulation factor deficiencies: 28%). In multivariable regression, we identified female sex, younger age, and higher body mass index, but not MBD diagnoses, bleeding score, or blood group O, associated with ID.
Conclusion
ID was common among MBDs, especially von Willebrand disease and female patients, but also in controls. Our data highlight the importance of assessing iron status in patients with MBDs, especially in young female individuals, regardless of the presence of bleeding symptoms.
轻中度出血性疾病和不明原因出血性疾病患者缺铁的发生率
背景:缺铁(ID)和缺铁贫血(IDA)通常是由慢性出血,尤其是月经大出血引起的,因此在轻中度出血性疾病(MBDs)患者中可能发生的频率很高。目的探讨轻中度出血性疾病及不明原因出血性疾病患者缺铁的情况。方法对来自维也纳出血生物库的MBD患者的铁状态进行前瞻性队列研究,并与年龄和性别匹配的健康对照进行比较。ID定义为铁蛋白≤30 μg/L,转铁蛋白饱和度≤16%,或包合时铁治疗。确诊为糖尿病的女性血红蛋白为12 g/dL,男性为13 g/dL。结果646名MBD患者和118名对照患者的ID和IDA发生率具有可比性,因为MBD患者中有250名(39%)患有ID, 40名(6%)患有IDA,而对照组中有37名(31%)患有ID, 6名(5%)患有IDA。多项检测校正前血管性血友病的ID率明显高于对照组(49%),而其他MBD诊断与对照组(不明原因出血性疾病:39%;血小板功能障碍:33%;凝血因子缺乏:28%)之间无显著差异。在多变量回归中,我们确定了女性性别、年龄较小和较高的体重指数,但没有发现MBD诊断、出血评分或O型血与ID相关。结论id在MBDs(尤其是血管性血友病和女性患者)中普遍存在,但在对照组中也存在。我们的数据强调了评估MBDs患者,特别是年轻女性患者铁状态的重要性,无论是否存在出血症状。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Research and Practice in Thrombosis and Haemostasis
Medicine-Hematology
CiteScore
5.60
自引率
13.00%
发文量
212
审稿时长
7 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


