The Scottish inflammatory prognostic score: A novel biomarker for predicting in-hospital mortality in acute heart failure with reduced ejection fraction
IF 2.6
4区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
Acute heart failure with reduced ejection fraction (AHF) remains a leading cause of ED visits, hospitalizations, and in-hospital mortality.
Objectives
To evaluate the prognostic utility of the Scottish Inflammatory Prognostic Score (SIPS) in patients with AHF.
Methods
This retrospective study analyzed 508 patients admitted with AHF between November 2022 and November 2024. The SIPS was calculated based on albumin and neutrophil levels. Clinical and laboratory parameters were compared between survivors and non-survivors to identify predictors of all-cause in-hospital mortality.
Results
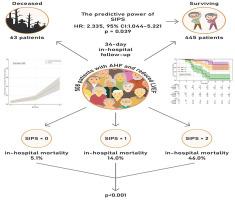
At a median follow-up of 10 days (range 4–28), 63 patients (12.4 %) died. The mean age of the study population was 63 years, with non-survivors being older on average. Multivariable Cox proportional regression analysis revealed high SIPS values (HR: 2.335, 95 % CI: 1.044 - 5.221, p = 0.039), advanced age, elevated NT-pro-BNP levels, chronic renal failure, and low serum sodium as independent predictors of in-hospital mortality. When patients were categorized by SIPS scores of 0, 1, and 2, the associated mortality rates were 5.1 %, 14.0 %, and 46.0 %, respectively (p < 0.001). Additionally, ROC curve analysis indicated that a SIPS threshold of 0.5 effectively predicted in-hospital mortality, demonstrating a sensitivity of 77 % and a specificity of 58 % (95 % CI: 0.661–0.803, p < 0.001).
Conclusions
This study is the first to analyze the association between SIPS and in-hospital mortality in patients with AHF. Integrating SIPS with other established risk factors may help improve the identification of high-risk AHF patients who could benefit from closer monitoring and intensified therapy, though further validation is warranted.
苏格兰炎症预后评分:预测急性心力衰竭伴射血分数降低的住院死亡率的一种新的生物标志物
急性心力衰竭伴射血分数降低(AHF)仍然是急诊科就诊、住院和住院死亡率的主要原因。目的评价苏格兰炎症预后评分(SIPS)在AHF患者中的预后价值。方法回顾性分析2022年11月至2024年11月收治的508例AHF患者。SIPS是根据白蛋白和中性粒细胞水平计算的。比较幸存者和非幸存者之间的临床和实验室参数,以确定全因住院死亡率的预测因素。结果中位随访10天(4 ~ 28天),63例(12.4%)患者死亡。研究人群的平均年龄为63岁,非幸存者的平均年龄更大。多变量Cox比例回归分析显示,高SIPS值(HR: 2.335, 95% CI: 1.044 ~ 5.221, p = 0.039)、高龄、NT-pro-BNP水平升高、慢性肾衰竭和低血清钠是院内死亡率的独立预测因素。当SIPS评分为0、1和2分时,相关死亡率分别为5.1%、14.0%和46.0% (p < 0.001)。此外,ROC曲线分析表明,SIPS阈值为0.5可以有效预测住院死亡率,灵敏度为77%,特异性为58% (95% CI: 0.661-0.803, p < 0.001)。结论本研究首次分析了SIPS与AHF患者住院死亡率之间的关系。将SIPS与其他已确定的危险因素相结合可能有助于提高对高危AHF患者的识别,这些患者可能受益于更密切的监测和强化治疗,但需要进一步验证。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Heart & Lung
医学-呼吸系统
CiteScore
4.60
自引率
3.60%
发文量
184
审稿时长
35 days
期刊介绍:
Heart & Lung: The Journal of Cardiopulmonary and Acute Care, the official publication of The American Association of Heart Failure Nurses, presents original, peer-reviewed articles on techniques, advances, investigations, and observations related to the care of patients with acute and critical illness and patients with chronic cardiac or pulmonary disorders.
The Journal''s acute care articles focus on the care of hospitalized patients, including those in the critical and acute care settings. Because most patients who are hospitalized in acute and critical care settings have chronic conditions, we are also interested in the chronically critically ill, the care of patients with chronic cardiopulmonary disorders, their rehabilitation, and disease prevention. The Journal''s heart failure articles focus on all aspects of the care of patients with this condition. Manuscripts that are relevant to populations across the human lifespan are welcome.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


