The Role of Peritoneal Interleukin-6 in Predicting Patient Survival on Peritoneal Dialysis
IF 5.7
2区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
Abstract
Introduction
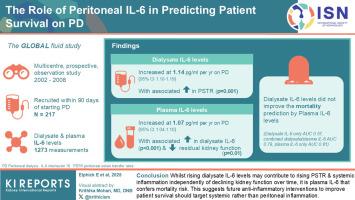
Systemic inflammation predicts cardiovascular events and mortality in patients on peritoneal dialysis (PD). Peritoneal inflammation potentially causes adverse outcomes by increasing peritoneal solute transfer rates (PSTRs); however, the extent to which it contributes to systemic inflammation is uncertain. We sought to quantify the longitudinal interrelationship between peritoneal and systemic inflammation, to understand whether peritoneal or systemic inflammation should be targeted to reduce mortality.
Methods
We used patients recruited to the GLOBAL Fluid Study (GFS) within 90 days of starting PD, with ≥ 3 longitudinal paired dialysate and plasma samples. These were assayed for dialysate and plasma interleukin (IL)-6 levels by electrochemiluminescence (Meso-Scale Discovery, Gaithersburg, MD). Linear mixed models and univariate or bivariate joint longitudinal survival modelling were used.
Results
Two hundred seventeen patients with 1273 measurements were included. Dialysate IL-6 levels increased with time (1.14 pg/ml/yr on PD, 95% confidence interval [CI]: 1.10–1.19), with an associated increase in PSTR (P = 0.001). Plasma IL-6 levels increased over time (1.07 pg/ml/yr on PD, 95% CI: 1.04–1.10), with an associated increase in dialysate IL-6 (P < 0.001) and reduction in residual kidney function (P = 0.01). Dialysate IL-6 levels estimated at any given time point weakly predicted mortality area under the curve (AUC: 0.57) and did not improve the prediction of mortality by plasma IL-6 (combined dialysate/plasma IL-6 AUC: 0.79, plasma IL-6 only AUC 0.81).
Conclusion
Although rising dialysate IL-6 levels may contribute to rising PSTR and increasing systemic inflammation independently of declining kidney function over time, it is plasma IL-6 that confers mortality risk. This suggests future antiinflammatory interventions to improve patient survival should target systemic rather than peritoneal inflammation.
腹膜白细胞介素-6在预测腹膜透析患者生存中的作用
全身性炎症预测腹膜透析(PD)患者的心血管事件和死亡率。腹膜炎症通过增加腹膜溶质转移速率(PSTRs)可能导致不良后果;然而,它对全身性炎症的影响程度尚不确定。我们试图量化腹膜和全身炎症之间的纵向相互关系,以了解腹膜或全身炎症是否应该以降低死亡率为目标。方法:我们招募了开始PD的90天内的全球流体研究(GFS)患者,具有≥3个纵向配对透析液和血浆样本。通过电化学发光检测透析液和血浆白细胞介素(IL)-6水平(Meso-Scale Discovery, Gaithersburg, MD)。采用线性混合模型和单变量或双变量关节纵向生存模型。结果共纳入1717例患者1273项测量数据。透析液IL-6水平随时间升高(PD时为1.14 pg/ml/yr, 95%可信区间[CI]: 1.10-1.19), PSTR相关升高(P = 0.001)。血浆IL-6水平随着时间的推移而升高(PD时为1.07 pg/ml/年,95% CI: 1.04-1.10),并伴有透析液IL-6升高(P < 0.001)和残余肾功能降低(P = 0.01)。在任何给定时间点估计的透析液IL-6水平弱预测曲线下的死亡率面积(AUC: 0.57),并没有改善血浆IL-6对死亡率的预测(透析液/血浆IL-6联合AUC: 0.79,血浆IL-6单独AUC 0.81)。结论虽然随着时间的推移,透析液IL-6水平升高可能导致PSTR升高和全身性炎症增加,而不是肾功能下降,但血浆IL-6是导致死亡风险的因素。这表明未来的抗炎干预措施,以提高患者的生存应该针对全身性而不是腹膜性炎症。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Kidney International Reports
Medicine-Nephrology
CiteScore
7.70
自引率
3.30%
发文量
1578
审稿时长
8 weeks
期刊介绍:
Kidney International Reports, an official journal of the International Society of Nephrology, is a peer-reviewed, open access journal devoted to the publication of leading research and developments related to kidney disease. With the primary aim of contributing to improved care of patients with kidney disease, the journal will publish original clinical and select translational articles and educational content related to the pathogenesis, evaluation and management of acute and chronic kidney disease, end stage renal disease (including transplantation), acid-base, fluid and electrolyte disturbances and hypertension. Of particular interest are submissions related to clinical trials, epidemiology, systematic reviews (including meta-analyses) and outcomes research. The journal will also provide a platform for wider dissemination of national and regional guidelines as well as consensus meeting reports.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


