Outcomes After Kidney Transplantation in Antiglomerular Basement Membrane Disease
IF 5.7
2区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
Abstract
Introduction
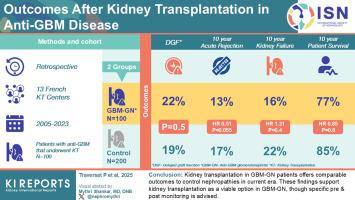
Goodpasture disease, or antiglomerular basement membrane (anti-GBM) disease, is a rare autoimmune disorder that often leads to end-stage kidney disease (ESKD). Although kidney transplantation (KT) is the preferred treatment, concerns exist about disease recurrence and graft outcomes in patients with GBM-associated glomerulonephritis (GBM-GN). This study aimed to evaluate posttransplant outcomes in patients with GBM-GN compared with matched controls.
Methods
This retrospective, multicenter study included 100 patients with anti-GBM who received KT between 2005 and 2023 in 13 French transplant centers, matched with 200 control recipients. We compared the incidence of delayed graft function (DGF), graft failure, relapse, acute rejection, and death between groups and analyzed risk factors using multivariable models.
Results
No significant differences in DGF incidence (22% vs. 19%, P = 0.5), graft survival (87% vs. 88% at 5 years, P = 0.4), or patient survival (93% vs. 89% at 5 years, P = 0.4) were found between patients with GBM-GN and controls. Patients with GBM-GN tended to have lower risk of acute rejection (hazard ratio [HR] = 0.51, 95% confidence interval: 0.25–1.02, P = 0.055). Only 1 patient with GBM-GN (1%) experienced disease relapse. Although patients with GBM-GN were waitlisted and transplanted later than controls, specific transplant timing was not associated with improved outcomes.
Conclusion
KT in patients with GBM-GN offers comparable outcomes to other nephropathies in the current era. Disease relapse is rare, even in the few patients with detectable antibodies pretransplantation. The lower incidence of acute rejection in the GBM-GN group warrants further investigation. These findings support KT as a viable option in patients with GBM-GN, though specific pre- and posttransplant monitoring is advised.
抗肾小球基底膜病肾移植后的预后
good牧草病,又称抗肾小球基底膜病(anti-GBM),是一种罕见的自身免疫性疾病,常导致终末期肾病(ESKD)。尽管肾移植(KT)是首选的治疗方法,但存在对gbm相关性肾小球肾炎(GBM-GN)患者疾病复发和移植结果的担忧。本研究旨在评估GBM-GN患者与匹配对照组的移植后预后。方法:这项回顾性的多中心研究纳入了2005年至2023年间在13个法国移植中心接受KT治疗的100例抗gbm患者,与200例对照患者相匹配。我们比较了两组间延迟移植功能(DGF)、移植失败、复发、急性排斥反应和死亡的发生率,并使用多变量模型分析了危险因素。结果GBM-GN患者与对照组在DGF发生率(22% vs. 19%, P = 0.5)、移植物存活率(87% vs. 88%, 5年,P = 0.4)或患者生存率(93% vs. 89%, 5年,P = 0.4)方面均无显著差异。GBM-GN患者的急性排斥反应风险较低(风险比[HR] = 0.51, 95%可信区间:0.25-1.02,P = 0.055)。只有1例(1%)GBM-GN复发。虽然GBM-GN患者的移植时间比对照组晚,但特定的移植时间与改善的结果无关。结论在当前时代,GBM-GN患者的kt与其他肾病患者的预后相当。疾病复发是罕见的,即使在少数患者检测抗体移植前。GBM-GN组较低的急性排斥发生率值得进一步研究。这些发现支持KT作为GBM-GN患者的可行选择,尽管建议进行特定的移植前和移植后监测。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Kidney International Reports
Medicine-Nephrology
CiteScore
7.70
自引率
3.30%
发文量
1578
审稿时长
8 weeks
期刊介绍:
Kidney International Reports, an official journal of the International Society of Nephrology, is a peer-reviewed, open access journal devoted to the publication of leading research and developments related to kidney disease. With the primary aim of contributing to improved care of patients with kidney disease, the journal will publish original clinical and select translational articles and educational content related to the pathogenesis, evaluation and management of acute and chronic kidney disease, end stage renal disease (including transplantation), acid-base, fluid and electrolyte disturbances and hypertension. Of particular interest are submissions related to clinical trials, epidemiology, systematic reviews (including meta-analyses) and outcomes research. The journal will also provide a platform for wider dissemination of national and regional guidelines as well as consensus meeting reports.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


