Nocturnal hypoxemia in infants with or without upper airway obstruction and its association with nocturnal pulse rate
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
Abstract
Objective
Nocturnal intermittent hypoxemia may enhance sympathetic nervous system activity. We aimed to assess the potential relationship of age-adjusted nocturnal pulse rate (% distance from 95th percentile for age-pulse rate index) with nocturnal oximetry parameters and their interaction with upper airway obstruction (UAO) presence.
Methods
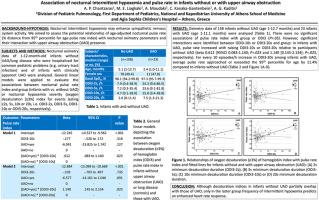
Nocturnal oximetry data of 1-12-month-old infants without UAO/lung disease who were hospitalized for common pediatric problems (e.g. urinary tract infection) and of infants with clinically apparent UAO were analyzed. General linear models were applied to evaluate associations of nocturnal pulse rate index with group (infants with vs. without UAO) or nocturnal hypoxemia severity (oxygen desaturation [≥3 %] index for events lasting ≥2s, ≥5s, ≥10s or ≥20s (ODI3-2s, ODI3-5s, ODI3-10s or ODI3-20s, respectively).
Results
Oximetry data of 158 infants without UAO (age 1–12.7 months) and 23 with UAO (age 1–11.1 months) were analyzed. There were no significant associations of pulse rate index with group or ODI3 (P > .05). However, significant interactions were identified between ODI3-10s or ODI3-20s and group: in infants with UAO, pulse rate increased with raising ODI3-10s or ODI3-20s compared to participants without UAO (beta .612 [95 %CI .083–1.140; P = .023 and 1.140 [.145–2.134]; P = .025, respectively). For every 10 episodes/h increase in ODI3-20s among infants with UAO, average pulse rate approached or exceeded the 95th percentile for age by 11.4 % compared to infants without UAO.
Conclusions
Despite overlap of desaturation indices values in infants without UAO and those with UAO, only in the latter, frequency of intermittent hypoxemia predicts an enhanced heart rate response.
伴有或不伴有上气道阻塞的婴儿夜间低氧血症及其与夜间脉搏率的关系
目的:夜间间歇性低氧血症可增强交感神经系统活动。我们的目的是评估年龄调整的夜间脉搏率(年龄脉搏率指数与第95百分位的距离百分比)与夜间血氧测定参数的潜在关系,以及它们与上呼吸道阻塞(UAO)存在的相互作用。方法分析1 ~ 12月龄无UAO/肺部疾病患儿因儿科常见病(如尿路感染)住院及临床明显UAO患儿的血氧测定数据。应用一般线性模型评价夜间脉搏率指数与组(有UAO与无UAO的婴儿)或夜间低氧血症严重程度(持续≥2s、≥5s、≥10s或≥20s(分别为ODI3-2s、ODI3-5s、ODI3-10s或ODI3-20s)事件的氧饱和度[≥3%]指数)的相关性。结果对158例无UAO(1 ~ 12.7月龄)和23例有UAO(1 ~ 11.1月龄)患儿的体测数据进行分析。脉搏率指数与组、ODI3无显著相关性(P > 0.05)。然而,odi3 -10或odi3 -20与组之间存在显著的相互作用:与没有UAO的参与者相比,患有UAO的婴儿脉搏率随着odi3 -10或odi3 -20的升高而增加。612 [95% ci .083-1.140;P = 0.023和1.140 [.145-2.134];P = 0.025)。与没有UAO的婴儿相比,UAO婴儿中ODI3-20s每增加10次/小时,平均脉搏率接近或超过年龄的第95百分位数11.4%。结论:尽管无UAO和有UAO的婴儿去饱和指数值有重叠,但只有后者,间歇性低氧血症的频率预示着心率反应的增强。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


