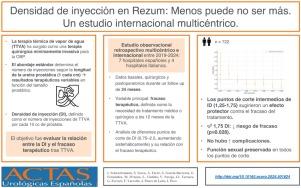
Densidad de inyección en Rezum®: menos puede no ser más. Un estudio internacional multicéntrico
IF 1.2
4区 医学
Q3 UROLOGY & NEPHROLOGY
引用次数: 0
Abstract
Introduction
Water vapor thermal therapy (WVTT) has emerged as a minimally invasive surgical therapy (MIST) for benign prostatic obstruction. However, the optimal number of intraprostatic injections remains debated. This study introduces injection density (ID), defined as the number of injections per 10 cc of prostate volume, to assess its impact on treatment failure after WVTT.
Methods
Multicentric retrospective study across 11 European centers, analysing patients who underwent WVTT between March 2019 and March 2024. Baseline, surgical, and postoperative data were collected during a 24 months follow-up. The primary outcome was treatment failure, defined as the need for medical or surgical intervention 12 months post-WVTT. Secondary outcomes included sexual function and postoperative complications. Logistic regression was performed across ID cut-off points from 0.75 to 2.5 injections per 10 cc.
Results
A total of 722 patients underwent WVTT with a mean age of 64 years and a mean prostate volume of 60 cc. Baseline Qmax was 8.0 ± 3.6 ml/s. Intermediate ID cut-off points (1.25-1.75) suggested a protective effect against treatment failure, with 1.75 being the first to reach statistical significance (p = 0.028). Higher ID cut-off points (2.00-2.50) maintained a protective effect, but only 2.25 reached significance (P=.024). No significant relationship was found between ID and complications. Sexual function remained stable across ID thresholds.
Conclusions
Optimizing ID during WVTT may improve success rates without increasing complications or negatively impacting sexual function. These findings support a volumetric approach over the traditional linear injection technique to enhance WVTT outcomes.
Rezum®的注射密度:少即是多。多中心国际研究
水蒸气热疗法(WVTT)已成为一种治疗良性前列腺阻塞的微创手术疗法(MIST)。然而,前列腺内注射的最佳次数仍有争议。本研究引入注射密度(ID),定义为每10cc前列腺体积注射的次数,以评估其对WVTT后治疗失败的影响。方法11个欧洲中心的多中心回顾性研究,分析2019年3月至2024年3月期间接受WVTT治疗的患者。在24个月的随访中收集基线、手术和术后数据。主要结局是治疗失败,定义为wvtt后12个月是否需要药物或手术干预。次要结局包括性功能和术后并发症。结果722例患者接受WVTT治疗,平均年龄64岁,平均前列腺体积60cc,基线Qmax为8.0±3.6 ml/s。中间ID分界点(1.25-1.75)提示对治疗失败有保护作用,1.75首先达到统计学意义(p = 0.028)。较高的ID分界点(2.00-2.50)维持了保护作用,但只有2.25达到显著性(P= 0.024)。ID与并发症无明显关系。性功能在ID阈值范围内保持稳定。结论在不增加并发症和不影响性功能的前提下,优化体外移植术的ID可提高手术成功率。这些发现支持容积法优于传统的线性注入技术,以提高WVTT的效果。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Actas urologicas espanolas
UROLOGY & NEPHROLOGY-
CiteScore
1.90
自引率
0.00%
发文量
98
审稿时长
46 days
期刊介绍:
Actas Urológicas Españolas is an international journal dedicated to urological diseases and renal transplant. It has been the official publication of the Spanish Urology Association since 1974 and of the American Urology Confederation since 2008. Its articles cover all aspects related to urology.
Actas Urológicas Españolas, governed by the peer review system (double blinded), is published online in Spanish and English. Consequently, manuscripts may be sent in Spanish or English and bidirectional free cost translation will be provided.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


