Electrocardiogram markers predicting ischemic stroke after acute coronary syndrome
IF 2.1
Q3 PERIPHERAL VASCULAR DISEASE
International Journal of Cardiology Cardiovascular Risk and Prevention
Pub Date : 2025-08-22
DOI:10.1016/j.ijcrp.2025.200500
引用次数: 0
Abstract
Background
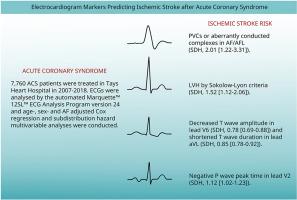
Patients with coronary artery disease (CAD) have increased risk of ischemic stroke (IS). Our aim was to screen for significant electrocardiogram (ECG) features for IS risk in patients treated for acute coronary syndrome (ACS).
Methods
This retrospective registry study is based on 7760 ACS patients treated in Tays Heart Hospital (2007–2018) with follow-up for incident IS until December 31st, 2020. ECGs recorded during ACSs were analysed by the Marquette™ 12SL™ ECG Analysis Program version 24. Preliminary screening for ECG features was conducted using age- and sex adjusted Cox regression analysis and corrected by multiple testing (Bonferroni method). Highly correlated variables were excluded from the final age-, sex- and atrial fibrillation (AF)/atrial flutter (AFL) adjusted Cox regression and subdistribution hazard (SDH) multivariable analyses.
Results
From 7760 patients, 489 (6.3 %) suffered IS during a median follow-up of 5.7 years (IQR 3.1–8.8). In the final multivariable model, the main risk factors were premature ventricular complexes (PVCs) or aberrantly conducted complexes in AF/AFL (SDH, 2.01 [1.22–3.31]), left ventricular (LV) hypertrophy (LVH) by Sokolow-Lyon criteria (SDH, 1.52 [1.12–2.06]), S wave amplitude in lead V4 (SDH, 1.13 [1.05–1.21]) and negative P wave peak time in lead V2 (SDH, 1.12 [1.02–1.23]). T wave amplitude in lead V6 (SDH, 0.78 [0.69–0.88]) and T wave duration in lead aVL (SDH, 0.85 [0.78–0.92]) showed an inverse association with IS risk. The continuous variables correspond to 1 SD.
Conclusions
ECG markers demonstrating LV dysfunction, LVH and atriopathy associate with IS risk after ACS, although external validation is still required.
心电图指标预测急性冠状动脉综合征后缺血性卒中
背景:冠心病(CAD)患者发生缺血性卒中(IS)的风险增加。我们的目的是筛查急性冠脉综合征(ACS)患者的重要心电图(ECG)特征。方法本回顾性登记研究基于2007-2018年在Tays心脏医院接受治疗的7760例ACS患者,随访至2020年12月31日。通过Marquette™12SL™ECG分析程序版本24分析ACSs期间记录的心电图。采用年龄和性别校正的Cox回归分析对心电图特征进行初步筛选,并通过多重检验(Bonferroni法)进行校正。高度相关的变量被排除在最终年龄、性别和心房颤动(AF)/心房扑动(AFL)校正Cox回归和亚分布风险(SDH)多变量分析之外。结果在中位随访5.7年(IQR 3.1-8.8)期间,7760例患者中,489例(6.3%)患有IS。在最终的多变量模型中,主要危险因素为房内/房内l室性早搏复合物(PVCs)或传导异常复合物(SDH, 2.01[1.22-3.31])、Sokolow-Lyon标准左室(LV)肥厚(LVH) (SDH, 1.52[1.12 - 2.06])、V4导联S波振幅(SDH, 1.13[1.05-1.21])和V2导联P波峰值时间(SDH, 1.12[1.02-1.23])。V6导联T波振幅(SDH, 0.78[0.69-0.88])和aVL导联T波持续时间(SDH, 0.85[0.78 - 0.92])与IS风险呈负相关。连续变量对应1个SD。结论secg标记显示左室功能障碍、左室h和心房病变与ACS后IS风险相关,但仍需要外部验证。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

International Journal of Cardiology Cardiovascular Risk and Prevention
Cardiology and Cardiovascular Medicine
CiteScore
3.00
自引率
0.00%
发文量
0
审稿时长
72 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


