Explaining the unknown: causal illness beliefs among people with epilepsy without identified cause
IF 2.3
3区 医学
Q2 BEHAVIORAL SCIENCES
引用次数: 0
Abstract
Objective
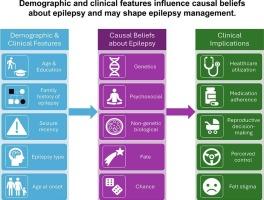
We explored the relations of demographic and clinical characteristics to causal illness beliefs (“attributions”) among people with epilepsy without identified non-genetic (acquired) cause.
Methods
We surveyed 644 patients treated at a comprehensive epilepsy center (2019–2022) and abstracted data from their medical records. Participants completed the revised Illness Perception Questionnaire, rating the likelihood of 17 possible causes of their epilepsy, and named what they believed was the most important cause in a free-response item. We collapsed causal attributions into five factors: genetics, psychosocial, non-genetic biological, fate, and chance. We assessed associations of causal attributions with demographic and clinical epilepsy characteristics using multivariate generalized linear and multinomial logistic regression models.
Results
Participants with a family history of epilepsy were more likely to endorse genetic causes (adjusted mean [aM] = 2.85) than were those without (aM = 2.14), p < 0.001. Those with a high school education or less (aM = 1.78) were more likely to endorse psychosocial causes (e.g., psychological distress) than were college graduates (aM = 1.46), p < 0.001. Participants whose last seizure was < 1 year ago were more likely to attribute their epilepsy to psychosocial causes (aM = 1.55) than were those whose last seizure was ≥ 1 year ago (aM = 1.33), p < 0.001. In the free-response item, the causes considered most important were: non-genetic biological (43.8 %), genetics (26.8 %), psychosocial (20.7 %), fate (6.0 %), and chance (2.7 %).
Significance
Demographic and clinical characteristics are associated with causal attributions of epilepsy. These relationships have implications for epilepsy management and treatment and suggest a need for improved patient-centered communication about epilepsy.
解释未知:病因不明的癫痫患者的病因信念
目的探讨未确定非遗传(获得性)病因的癫痫患者的人口学特征和临床特征与病因信念(“归因”)的关系。方法对2019-2022年在某综合癫痫中心治疗的644例患者进行调查,并从其病历中提取数据。参与者完成了修订后的疾病认知问卷,对17种可能导致癫痫的原因进行了可能性评级,并在一个自由回答项目中列出了他们认为最重要的原因。我们将因果归因归结为五个因素:遗传、社会心理、非遗传生物、命运和机会。我们使用多元广义线性和多项逻辑回归模型评估了因果归因与人口统计学和临床癫痫特征的关联。结果有癫痫家族史的参与者比没有癫痫家族史的参与者更容易认同遗传原因(调整后的平均值[aM] = 2.85), p < 0.001。与大学毕业生(aM = 1.46)相比,高中学历或更低学历(aM = 1.78)的人更有可能认同心理社会原因(如心理困扰),p < 0.001。最后一次癫痫发作为1年前的参与者比最后一次癫痫发作≥1年前的参与者(aM = 1.55)更有可能将其癫痫归因于心理社会原因(p < 0.001)。在自由反应项目中,被认为最重要的原因是:非遗传生物(43.8%)、遗传(26.8%)、社会心理(20.7%)、命运(6.0%)和机会(2.7%)。人口统计学和临床特征与癫痫的因果归因有关。这些关系对癫痫的管理和治疗有影响,并提示需要改善以患者为中心的癫痫沟通。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Epilepsy & Behavior
医学-行为科学
CiteScore
5.40
自引率
15.40%
发文量
385
审稿时长
43 days
期刊介绍:
Epilepsy & Behavior is the fastest-growing international journal uniquely devoted to the rapid dissemination of the most current information available on the behavioral aspects of seizures and epilepsy.
Epilepsy & Behavior presents original peer-reviewed articles based on laboratory and clinical research. Topics are drawn from a variety of fields, including clinical neurology, neurosurgery, neuropsychiatry, neuropsychology, neurophysiology, neuropharmacology, and neuroimaging.
From September 2012 Epilepsy & Behavior stopped accepting Case Reports for publication in the journal. From this date authors who submit to Epilepsy & Behavior will be offered a transfer or asked to resubmit their Case Reports to its new sister journal, Epilepsy & Behavior Case Reports.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


