High- and intermediate-risk pulmonary embolism in pediatric tertiary care centers in the Netherlands
IF 3.4
3区 医学
Q2 HEMATOLOGY
Research and Practice in Thrombosis and Haemostasis
Pub Date : 2025-08-01
DOI:10.1016/j.rpth.2025.102972
引用次数: 0
Abstract
Background
Pulmonary embolism (PE) response teams are increasingly used in adult care to improve severe PE management. Understanding the epidemiology, treatment, and outcomes of severe PE in children is crucial to assessing the need for pediatric PE response teams in the Netherlands.
Objectives
To evaluate the incidence, management, and short-term outcomes of severe PE in Dutch pediatric patients.
Methods
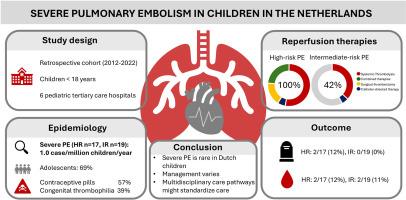
This retrospective cohort study included children (0-18 years) diagnosed with high- and intermediate-risk PE between 2012 and 2022 across 6 pediatric tertiary care centers in the Netherlands.
Results
Among 172 PE patients, 17 (10%) had high-risk PE and 19 (11%) had intermediate-risk PE. The annual PE incidence was estimated at 1.0 case per million children, predominantly affecting adolescents. Common symptoms included dyspnea (90%) and tachypnea (75%). Major risk factors were oral contraceptive use (57%) and congenital thrombophilia (39%). In the high-risk group, 100% underwent reperfusion therapy, including systemic thrombolysis (n = 13), surgical thrombectomy (n = 3), and catheter-directed therapy (CDT; n = 1). Four systemic thrombolysis failures required further intervention (3 CDT and 1 surgical thrombectomy). Major bleeding occurred in 2 patients (12%), and 2 (12%) suffered PE-related deaths. Among intermediate-risk patients, 42% received reperfusion therapy (7 systemic thrombolysis and 1 CDT), with major bleeding in 2 (11%) and no deaths. Postdischarge treatment included low-molecular-weight heparin (n = 10), vitamin K antagonists (n = 7), and direct oral anticoagulants (n = 17).
Conclusion
Severe PE is rare in Dutch children. The variation in indications and reperfusion strategies highlights the need for national, multidisciplinary care pathways to standardize management and improve outcomes.
荷兰儿科三级护理中心的高、中危肺栓塞
背景肺栓塞(PE)反应小组越来越多地用于成人护理,以改善严重的PE管理。了解儿童严重PE的流行病学、治疗和结果对于评估荷兰儿童PE反应小组的需求至关重要。目的评价荷兰儿童重症PE的发生率、治疗和短期预后。方法:本回顾性队列研究纳入了荷兰6个儿科三级保健中心2012年至2022年间诊断为高危和中危PE的儿童(0-18岁)。结果172例PE患者中,高危PE 17例(10%),中危PE 19例(11%)。每年的PE发病率估计为每百万儿童1.0例,主要影响青少年。常见症状包括呼吸困难(90%)和呼吸急促(75%)。主要危险因素是口服避孕药(57%)和先天性血栓形成(39%)。高危组100%接受再灌注治疗,包括全身溶栓(n = 13)、手术取栓(n = 3)和导管定向治疗(CDT; n = 1)。4例全身溶栓失败需要进一步干预(3例CDT和1例手术取栓)。2例(12%)患者发生大出血,2例(12%)患者发生pe相关死亡。在中危患者中,42%接受了再灌注治疗(7例全身性溶栓和1例CDT), 2例(11%)发生大出血,无死亡。出院后治疗包括低分子肝素(n = 10)、维生素K拮抗剂(n = 7)和直接口服抗凝剂(n = 17)。结论荷兰儿童严重PE少见。适应症和再灌注策略的变化突出了国家多学科护理途径的需求,以规范管理和改善结果。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Research and Practice in Thrombosis and Haemostasis
Medicine-Hematology
CiteScore
5.60
自引率
13.00%
发文量
212
审稿时长
7 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


