Prognostic value of CT-PCI and CA-125 changes following neoadjuvant chemotherapy in advanced epithelial ovarian cancer: A retrospective study from Vietnam
IF 1.3
Q3 OBSTETRICS & GYNECOLOGY
引用次数: 0
Abstract
Introduction
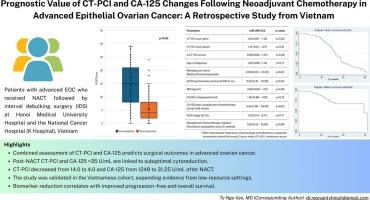
This study aimed to evaluate the prognostic significance of CT-based Peritoneal Cancer Index (CT-PCI) scores and serum CA-125 levels, assessed before and after neoadjuvant chemotherapy (NACT), in relation to surgical outcomes and survival among patients with advanced-stage epithelial ovarian cancer (EOC).
Methods
This retrospective study included 96 patients with advanced EOC who received NACT followed by interval debulking surgery (IDS) at Hanoi Medical University Hospital and the National Cancer Hospital (K Hospital), Vietnam, between 2019 and 2024. CT-PCI scores and CA-125 levels were assessed both pre- and post-NACT. The associations between these changes and surgical outcomes, particularly optimal cytoreduction, were analyzed.
Results
The mean age was 59.17 years (SD = 9.78), with 94.8 % of patients diagnosed with high-grade serous carcinoma and 51.0 % classified as FIGO stage IIIC. Median CT-PCI scores decreased from 14.0 (IQR: 7.0–19.0) to 4.0 (IQR: 2.0–8.0), and median CA-125 levels declined from 1248 U/ml (IQR: 389–2855) to 31.25 U/ml (IQR: 16.75–147.3) post-treatment (both p < 0.01). Optimal cytoreduction was achieved in 84.4 % of cases. Post-NACT CT-PCI scores and CA-125 levels > 35 U/ml were significantly associated with suboptimal cytoreduction (cOR = 1.15, 95 % CI: 1.03–1.27, p = 0.01; and cOR = 5.26, 95 % CI: 1.38–33.00, p = 0.02, respectively). Median progression-free survival was 20.5 months; median overall survival was 36.7 months.
Conclusion
Post-treatment CT-PCI scores and CA-125 levels are valuable prognostic indicators in advanced epithelial ovarian cancer. Their reduction following NACT correlates significantly with improved progression-free and overall survival. These findings support their potential role in informing clinical decision-making and tailoring personalized treatment strategies.
来自越南的一项回顾性研究:晚期上皮性卵巢癌新辅助化疗后CT-PCI和CA-125变化的预后价值
本研究旨在评估基于ct的腹膜癌指数(CT-PCI)评分和血清CA-125水平的预后意义,在新辅助化疗(NACT)前后评估,与晚期上皮性卵巢癌(EOC)患者的手术结局和生存有关。方法回顾性研究包括2019年至2024年在越南河内医科大学医院和国立肿瘤医院(K医院)接受NACT术后间歇减瘤手术(IDS)的96例晚期EOC患者。CT-PCI评分和CA-125水平分别在nact前后进行评估。分析了这些变化与手术结果之间的关系,特别是最佳的细胞减少。结果平均年龄59.17岁(SD = 9.78), 94.8%的患者诊断为高级别浆液性癌,51.0%的患者诊断为FIGO IIIC期。治疗后CT-PCI评分中位数从14.0 (IQR: 7.0-19.0)降至4.0 (IQR: 2.0-8.0), CA-125水平中位数从1248 U/ml (IQR: 389-2855)降至31.25 U/ml (IQR: 16.75-147.3) (p均为0.01)。84.4%的病例达到最佳的细胞减少率。nact后CT-PCI评分和CA-125水平(gt; 35 U/ml)与亚理想细胞减少显著相关(cOR = 1.15, 95% CI: 1.03-1.27, p = 0.01; cOR = 5.26, 95% CI: 1.38-33.00, p = 0.02)。中位无进展生存期为20.5个月;中位总生存期为36.7个月。结论CT-PCI治疗后评分和CA-125水平是晚期上皮性卵巢癌有价值的预后指标。NACT后的减少与无进展和总生存期的改善显著相关。这些发现支持了它们在告知临床决策和定制个性化治疗策略方面的潜在作用。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Gynecologic Oncology Reports
OBSTETRICS & GYNECOLOGY-
CiteScore
2.00
自引率
0.00%
发文量
183
审稿时长
41 days
期刊介绍:
Gynecologic Oncology Reports is an online-only, open access journal devoted to the rapid publication of narrative review articles, survey articles, case reports, case series, letters to the editor regarding previously published manuscripts and other short communications in the field of gynecologic oncology. The journal will consider papers that concern tumors of the female reproductive tract, with originality, quality, and clarity the chief criteria of acceptance.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


