When the victim becomes the villain: Platelets as drivers of immune dysregulation in ITP
IF 3.6
Q2 IMMUNOLOGY
引用次数: 0
Abstract
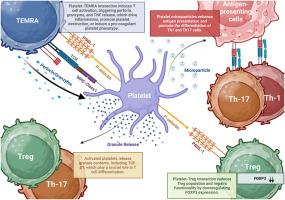
Immune thrombocytopenia (ITP) is a heterogeneous autoimmune disorder characterized by immune-mediated destruction of platelets and impaired platelet production. Although autoantibodies have historically been central to the understanding of ITP, current evidence demonstrates that its pathogenesis extends well beyond humoral mechanisms to involve complex dysregulation of both innate and adaptive immune responses. Multiple immune pathways—including autoreactive B and T cells, dendritic cell activation, and regulatory T cell deficiency—contribute to disease onset, progression, and chronicity. Moreover, ITP encompasses a broad spectrum of clinical and immunological subtypes, including primary idiopathic forms and secondary ITP associated with autoimmune diseases, infections, and inborn errors of immunity. This review offers a novel perspective on ITP pathogenesis, emphasizing the active immunoregulatory role of platelets as contributors to immune dysregulation. Far from being passive targets, platelets in ITP actively shape immune responses through crosstalk with immune cells, particularly CD4+ T helper (Th) and CD8+ cytotoxic T cells. This interaction, primarily mediated via the P-selectin–PSGL-1 axis, promotes Th1/Th17 polarization, enhances autoantibody production, and accelerates platelet destruction. In parallel, platelet-derived microparticles (PMPs) act as potent immune effectors by delivering pro-inflammatory cytokines and autoantigens that sustain chronic immune activation. Prolonged platelet activation also gives rise to a distinct subpopulation known as “hairy platelets”—exhausted, granule-depleted cells with altered surface phenotypes and sustained pro-inflammatory potential. Although functionally exhausted in terms of coagulation, these platelets retain immunostimulatory capacity through persistent phosphatidylserine exposure and cytokine release. By reframing platelets as active participants in the pathogenesis of ITP, this review proposes that targeting platelet activation, platelet–T cell interactions, and PMP release may represent innovative therapeutic strategies. Such approaches could offer more precise and personalized treatment options, particularly for patients with chronic or refractory disease, by restoring immune balance and improving long-term outcomes.
当受害者变成恶棍:血小板作为ITP免疫失调的驱动因素
免疫性血小板减少症(ITP)是一种异质性自身免疫性疾病,其特征是免疫介导的血小板破坏和血小板产生受损。虽然自身抗体历来是理解ITP的核心,但目前的证据表明,其发病机制远远超出体液机制,涉及先天和适应性免疫反应的复杂失调。多种免疫途径——包括自身反应性B细胞和T细胞、树突状细胞激活和调节性T细胞缺陷——有助于疾病的发病、进展和慢性。此外,ITP包括广泛的临床和免疫学亚型,包括原发性特发性形式和与自身免疫性疾病、感染和先天性免疫错误相关的继发性ITP。这篇综述为ITP的发病机制提供了一个新的视角,强调血小板在免疫失调中的积极免疫调节作用。ITP中的血小板远非被动靶标,而是通过与免疫细胞,特别是CD4+ T辅助细胞(Th)和CD8+细胞毒性T细胞的串扰,主动塑造免疫反应。这种相互作用主要通过p -选择素- psgl -1轴介导,促进Th1/Th17极化,增强自身抗体的产生,加速血小板破坏。与此同时,血小板衍生微粒(pmp)通过传递促炎细胞因子和自身抗原作为有效的免疫效应器,维持慢性免疫激活。长时间的血小板激活也会产生一种独特的亚群,称为“毛血小板”——耗尽的、颗粒耗尽的细胞,表面表型改变,具有持续的促炎潜力。尽管在凝血方面功能衰竭,这些血小板通过持续的磷脂酰丝氨酸暴露和细胞因子释放保持免疫刺激能力。通过将血小板重新定义为ITP发病机制的积极参与者,本文提出靶向血小板活化、血小板- t细胞相互作用和PMP释放可能代表创新的治疗策略。这种方法可以通过恢复免疫平衡和改善长期预后,提供更精确和个性化的治疗选择,特别是对慢性或难治性疾病患者。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Translational Autoimmunity
Medicine-Immunology and Allergy
CiteScore
7.80
自引率
2.60%
发文量
33
审稿时长
55 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


