Elucidating the causal role of age of menarche, adiposity, lipid fractions, and blood pressure upon cardiovascular disease: a multivariable Mendelian randomization study
IF 3.4
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
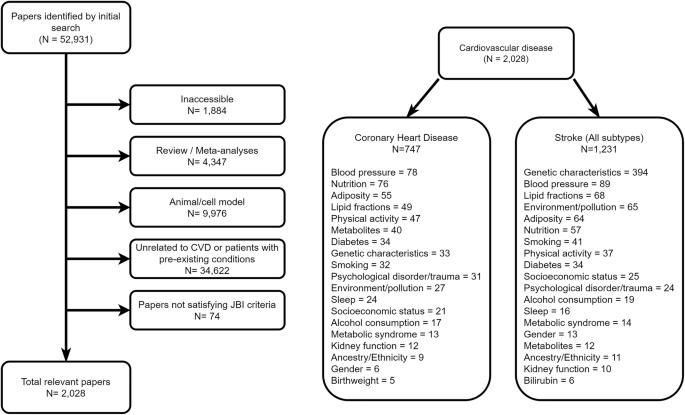
This study explores the causal role of multiple correlated risk factors in coronary heart disease (CHD) and ischemic stroke, using Mendelian randomization (MR) analyses with GWAS summary data from both prevalent and incident stroke cases. Thirteen candidate risk factors were considered, including age at menarche, adiposity, lipid fractions, blood pressure, and smoking. Univariable MR identified seven exposures significantly associated with CHD risk, including BMI, blood pressure, LDL, triglycerides, type-II diabetes, and smoking. Notably, HDL showed a protective effect (OR = 0.77, 95% CI: 0.72–0.83), while type-II diabetes was positively associated with CHD (OR = 1.10, 95% CI: 1.05–1.16). For ischemic stroke subtypes, diastolic and systolic blood pressure showed consistent effects across both small vessel and large artery stroke (e.g., DBP OR = 2.27, 95% CI: 1.77–2.89 for small vessel stroke), and HDL again demonstrated protective effects. Multivariable MR (MVMR) further confirmed these associations, though estimates were attenuated. In summary, both univariable and MVMR analyses identified robust associations of lipid fractions and blood pressure with cardiovascular outcomes, highlighting their importance in CHD and ischemic stroke risk across multiple stroke subtypes.
阐明月经初潮年龄、肥胖、脂质分数和血压对心血管疾病的因果作用:一项多变量孟德尔随机化研究
本研究采用孟德尔随机化(MR)分析方法,结合GWAS对流行和偶发卒中病例的汇总数据,探讨了多种相关危险因素在冠心病(CHD)和缺血性卒中中的因果作用。考虑了13个候选危险因素,包括初潮年龄、肥胖、脂质分数、血压和吸烟。单变量MR确定了7种与冠心病风险显著相关的暴露,包括BMI、血压、低密度脂蛋白、甘油三酯、ii型糖尿病和吸烟。值得注意的是,HDL具有保护作用(OR = 0.77, 95% CI: 0.72-0.83),而ii型糖尿病与冠心病呈正相关(OR = 1.10, 95% CI: 1.05-1.16)。对于缺血性卒中亚型,舒张压和收缩压在小血管和大动脉卒中中均表现出一致的影响(例如,小血管卒中的DBP OR = 2.27, 95% CI: 1.77-2.89), HDL再次表现出保护作用。多变量MR (MVMR)进一步证实了这些关联,尽管估计值有所降低。总之,单变量分析和MVMR分析都确定了脂质组分和血压与心血管结局的强大关联,强调了它们在多种卒中亚型的冠心病和缺血性卒中风险中的重要性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


