Systemic lupus erythematosus in critical care: A systematic review of ICU outcomes and management
IF 8.3
1区 医学
Q1 IMMUNOLOGY
引用次数: 0
Abstract
Background
Systemic lupus erythematosus (SLE) often progresses to critical illness requiring intensive care unit (ICU) admission, yet contemporary data on outcomes, prognostic factors, and therapeutic approaches are scattered.
Objective
To synthesize recent evidence on causes of ICU admission, mortality predictors, and management strategies in adult SLE.
Methods
A PRISMA-compliant search of PubMed, Web of Science and Cochrane Library (inception–31 December 2024) retrieved studies enrolling adults (≥18 years) with confirmed SLE treated in ICUs. Two reviewers independently selected articles and extracted data; methodological heterogeneity precluded meta-analysis, so results were narratively synthesized.
Results
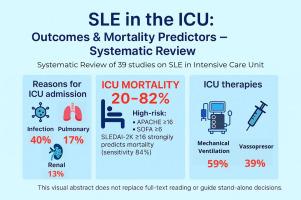
Thirty-nine studies met the criteria. Infection (40 %), pulmonary involvement (17 %) and renal flares (13 %) were the most common admission triggers. Reported ICU mortality ranged from 20 % to 82 % but rose sharply when baseline Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) exceeded 16, approximating 80 % mortality (sensitivity 84 %, specificity 90 %) and outperforming Acute Physiology and Chronic Health Evaluation (APACHE) II and Sequential Organ Failure Assessment (SOFA) in discriminating survivors. Additional independent predictors were APACHE II > 16, need for mechanical ventilation, renal replacement therapy and vasopressor support. Mechanical ventilation (59 %) and vasoactive agents (39 %) were the predominant ICU interventions. Immunomodulatory management was heterogeneous: high-dose corticosteroids and cyclophosphamide were ubiquitous, whereas mycophenolate, antimalarials, intravenous immunoglobulin, plasmapheresis, and extracorporeal membrane oxygenation were reserved for selected scenarios.
Conclusions
Early recognition of poor prognostic factors and prompt ICU admission are essential to improving outcomes in SLE.
重症监护中的系统性红斑狼疮:ICU结局和管理的系统回顾。
背景:系统性红斑狼疮(SLE)经常发展为需要重症监护病房(ICU)住院的危重疾病,但目前关于结果、预后因素和治疗方法的数据分散。目的:综合有关成人SLE住院原因、死亡率预测因素和治疗策略的最新证据。方法:检索PubMed、Web of Science和Cochrane Library(开始- 2024年12月31日)的符合prisma标准的研究,检索了在icu中确诊SLE的成人(≥18 岁)。两位审稿人独立选择文章和提取数据;方法学异质性排除了meta分析,因此结果是叙述性综合的。结果:39项研究符合标准。感染(40 %)、肺部受累(17 %)和肾脏耀斑(13 %)是最常见的入院诱因。报告的ICU死亡率范围为20 %至82 %,但当基线系统性红斑狼疮疾病活动指数2000 (sledai2 K)超过16时,死亡率急剧上升,接近80 %(敏感性84 %,特异性90 %),在区分幸存者方面优于急性生理和慢性健康评估(APACHE) II和顺序器官衰竭评估(SOFA)。其他独立预测因子为APACHE II > 16、需要机械通气、肾脏替代治疗和血管加压药物支持。机械通气(59 %)和血管活性药物(39 %)是ICU的主要干预措施。免疫调节管理是异质性的:大剂量皮质类固醇和环磷酰胺普遍存在,而霉酚酸盐、抗疟药、静脉免疫球蛋白、血浆置换和体外膜氧合则保留用于特定情况。结论:早期识别不良预后因素并及时进入ICU治疗对于改善SLE预后至关重要。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Autoimmunity reviews
医学-免疫学
CiteScore
24.70
自引率
4.40%
发文量
164
审稿时长
21 days
期刊介绍:
Autoimmunity Reviews is a publication that features up-to-date, structured reviews on various topics in the field of autoimmunity. These reviews are written by renowned experts and include demonstrative illustrations and tables. Each article will have a clear "take-home" message for readers.
The selection of articles is primarily done by the Editors-in-Chief, based on recommendations from the international Editorial Board. The topics covered in the articles span all areas of autoimmunology, aiming to bridge the gap between basic and clinical sciences.
In terms of content, the contributions in basic sciences delve into the pathophysiology and mechanisms of autoimmune disorders, as well as genomics and proteomics. On the other hand, clinical contributions focus on diseases related to autoimmunity, novel therapies, and clinical associations.
Autoimmunity Reviews is internationally recognized, and its articles are indexed and abstracted in prestigious databases such as PubMed/Medline, Science Citation Index Expanded, Biosciences Information Services, and Chemical Abstracts.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


