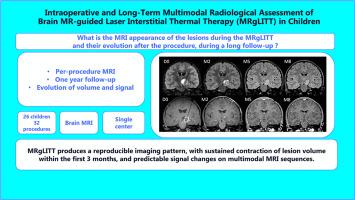
Intraoperative and long-term multimodal radiological assessment of brain MR-guided laser interstitial thermal therapy (MRgLITT) in children
IF 3.3
3区 医学
Q2 CLINICAL NEUROLOGY
引用次数: 0
Abstract
Objectives
Magnetic resonance-guided laser interstitial thermal therapy (MRgLITT) has emerged as a minimally invasive alternative for drug-resistant epilepsy and pediatric brain tumors, particularly in deep-seated lesions where open surgery presents significant risks. However, the multimodal imaging characteristics of lesions during and after MRgLITT remain underexplored. This study aims to describe the MRI features of MRgLITT-treated lesions in pediatric patients both intraoperatively and during long-term follow-up.
Methods
We conducted a retrospective analysis of 26 pediatric patients(32 procedures) treated using MRgLITT, including focal cortical dysplasias, low-grade tumors and hamartomas. Imaging acquisition included preoperative, intraoperative, and postoperative MRI with advanced sequences(T1-weighted, FLAIR, DWI, ASL perfusion, and MR spectroscopy). Lesion evolution was assessed over a one-year follow-up period.
Results
Intraoperatively, lesions showed a rim of high signal on DWI and on post-contrast T1-weighted images, a lactate peak on MR spectroscopy, and the majority of them had peripheral high signal on FLAIR associated with a low signal core and increased CBF on ASL. During follow-up, lesions may increase in size in the first days or weeks, then decrease in size mainly in the first 3 months and tend to stabilize at 9 months, with persistent gliotic changes on FLAIR sequences. Contrast enhancement resolved in epilepsy-related lesions, but small areas remained in most tumors without correlation with progression.
Conclusion
MRgLITT results in a predictable pattern of imaging changes, with lesion contraction occurring primarily within the first 3 months. Understanding these radiological markers is essential for optimizing post-procedure management and treatment decisions in pediatric epilepsies and tumors.
儿童脑磁共振引导的激光间质热治疗术中及长期多模态放射学评价。
目的:磁共振引导的激光间质热疗法(MRgLITT)已成为治疗耐药癫痫和儿童脑肿瘤的一种微创替代方法,特别是在开放性手术存在重大风险的深部病变中。然而,MRgLITT期间和之后病变的多模态成像特征仍未得到充分探讨。本研究旨在描述mrglitt治疗的儿科患者术中和长期随访期间病变的MRI特征。方法:我们对26例使用MRgLITT治疗的儿童患者(32种手术)进行了回顾性分析,包括局灶性皮质发育不良、低级别肿瘤和错构瘤。成像采集包括术前、术中和术后MRI先进序列(t1加权、FLAIR、DWI、ASL灌注和MR光谱)。在一年的随访期间评估病变演变。结果:术中,病变在DWI和造影后t1加权图像上显示高信号边缘,MR光谱上显示乳酸峰,大多数病变在FLAIR上呈外周高信号伴低信号核心,ASL上CBF增加。在随访期间,病变可能在最初的几天或几周内增大,然后主要在前3个月减小,并在9个月时趋于稳定,FLAIR序列显示持续的胶质样变化。对比增强在癫痫相关病变中消失,但在大多数肿瘤中仍存在小区域,与进展无关。结论:MRgLITT显示可预测的影像学改变模式,病变收缩主要发生在前3个月内。了解这些放射学标记对于优化小儿癫痫和肿瘤的术后管理和治疗决策至关重要。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Neuroradiology
医学-核医学
CiteScore
6.10
自引率
5.70%
发文量
142
审稿时长
6-12 weeks
期刊介绍:
The Journal of Neuroradiology is a peer-reviewed journal, publishing worldwide clinical and basic research in the field of diagnostic and Interventional neuroradiology, translational and molecular neuroimaging, and artificial intelligence in neuroradiology.
The Journal of Neuroradiology considers for publication articles, reviews, technical notes and letters to the editors (correspondence section), provided that the methodology and scientific content are of high quality, and that the results will have substantial clinical impact and/or physiological importance.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


