Association of Left Atrial Dysfunction with Pulmonary Hemodynamics and Cardiovascular Outcomes in Patients with Systemic Sclerosis
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
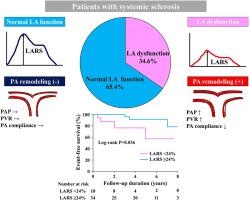
Left atrial (LA) reservoir strain (LARS) is emerging as an early marker of cardiac remodelling, providing significant prognostic information. The present study investigated the prevalence of LA dysfunction and its association with pulmonary hemodynamics and cardiovascular (CV) outcomes in systemic sclerosis (SSc) patients.
Methods
We included 52 patients who had SSc without structural cardiac disease. All patients underwent 2-dimensional transthoracic echocardiography and right heart catheterization. LARS was assessed by using speckle-tracking analysis. The study outcome was a composite of heart failure or pulmonary hypertension (PH)–related hospitalization, lung transplantation, and CV death.
Results
Abnormal LARS (< 24%) was present in 18 patients (34.6%). Despite the similar prevalence of PH between groups with abnormal vs normal LARS (P = 0.322), patients with LA dysfunction had significantly higher pulmonary vascular resistance (3.5 Wood Units [1.9-5.2] vs 2.0 Wood Units [1.3-2.9], P = 0.029) and reduced pulmonary artery compliance (2.4 [2.1-4.1] ml/mm Hg vs. 3.9 [2.5-5.0] ml/mm Hg, p=0.024) than those with normal LARS. During a median follow-up of 3.2 years, patients with LA dysfunction displayed worse event-free survival than their counterparts (log-rank P = 0.036). The combination of LA function and PH status provided better risk stratification for composite CV outcome, as the highest incidence of adverse outcome was observed in patients with LA dysfunction and PH (40.0%), followed by those with LA dysfunction or PH alone (13.6%), and finally those without LA dysfunction and PH (0%, P = 0.008).
Conclusions
LA dysfunction was related to unfavourable pulmonary artery remodelling and adverse outcomes in SSc patients without structural cardiac disease.
系统性硬化症患者左心房功能障碍与肺血流动力学和心血管预后的关系
背景:左心房(LA)储层应变(LARS)正成为心脏重构的早期标志物,提供了重要的预后信息。本研究调查了系统性硬化症(SSc)患者LA功能障碍的患病率及其与肺血流动力学和心血管(CV)结局的关系。方法纳入52例无结构性心脏病的SSc患者。所有患者均行二维经胸超声心动图和右心导管检查。利用斑点跟踪分析评估LARS。研究结果是心力衰竭或肺动脉高压(PH)相关住院、肺移植和CV死亡的综合结果。结果LARS异常(<;24%), 18例(34.6%)。尽管LARS异常组与正常组之间的PH患病率相似(P = 0.322),但与LARS正常组相比,LA功能障碍患者的肺血管阻力明显更高(3.5 Wood Units [1.9-5.2] vs 2.0 Wood Units [1.3-2.9], P = 0.029),肺动脉顺应性明显降低(2.4 [2.1-4.1]ml/mm Hg vs 3.9 [2.5-5.0] ml/mm Hg, P =0.024)。在中位随访3.2年期间,LA功能障碍患者的无事件生存率比对照组更差(log-rank P = 0.036)。LA功能和PH状态的联合为复合CV结局提供了更好的风险分层,因为不良结局发生率最高的是LA功能障碍和PH患者(40.0%),其次是LA功能障碍或PH单独患者(13.6%),最后是没有LA功能障碍和PH的患者(0%,P = 0.008)。结论在无结构性心脏病的SSc患者中,sla功能障碍与不利的肺动脉重构和不良结局有关。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

CJC Open
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
3.30
自引率
0.00%
发文量
143
审稿时长
60 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


