Combined Flt3L and CD40 agonism restores dendritic cell–driven T cell immunity in pancreatic cancer
IF 16.3
1区 医学
Q1 IMMUNOLOGY
引用次数: 0
Abstract
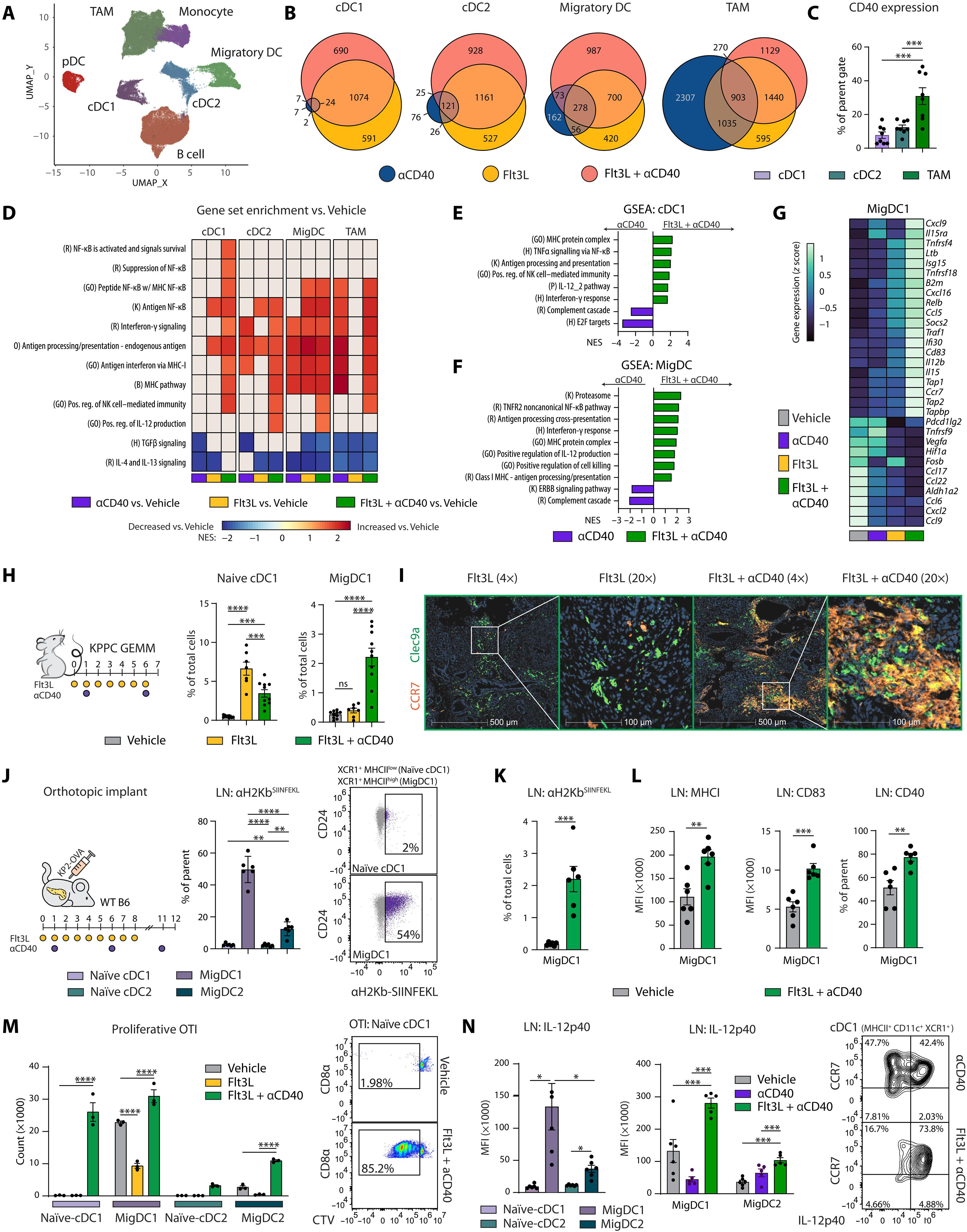
T cell–directed immunotherapies have largely failed to slow progression of pancreatic ductal adenocarcinoma (PDAC) because of poor tumor antigenicity and an immunosuppressive tumor microenvironment. We hypothesized that conventional dendritic cell (cDC) suppression in PDAC may further impair tumor immunity. We found that low tissue expression of Fms-like tyrosine kinase 3 ligand (Flt3L) partially underlies cDC deficits. Treatment with systemic Flt3L and CD40 agonists restored cDC number and function in murine models and clinical trial samples from patients with PDAC. CD40 agonism alone did not fully activate cDCs; however, when combined with Flt3L, dual therapy triggered a cDC-driven type I immune response characterized by T cell infiltration, interleukin-12 production, and reciprocal interferon-γ (IFN-γ) responses. In mice, cDC1s were responsible for CD8+ T cell expansion, and in turn, T cell–derived IFN-γ enhanced cDC1 survival. Nevertheless, Flt3L and CD40 agonism increased regulatory T cells through the activation of cDC2s, dampening immunity. These findings advocate further exploration of DC-centered approaches to enhance antitumor immunity in PDAC.
Flt3L和CD40联合激动作用恢复胰腺癌树突状细胞驱动的T细胞免疫
由于肿瘤抗原性差和免疫抑制肿瘤微环境,T细胞定向免疫疗法在很大程度上未能减缓胰腺导管腺癌(PDAC)的进展。我们假设PDAC中传统的树突状细胞(cDC)抑制可能进一步损害肿瘤免疫。我们发现fms样酪氨酸激酶3配体(Flt3L)的低组织表达是cDC缺陷的部分原因。在小鼠模型和PDAC患者的临床试验样本中,全身性Flt3L和CD40激动剂治疗可恢复cDC数量和功能。单独使用CD40激动剂不能完全激活cdc;然而,当与Flt3L联合使用时,双重治疗引发了以T细胞浸润、白细胞介素-12产生和相互干扰素-γ (IFN-γ)反应为特征的cdc驱动的I型免疫反应。在小鼠中,cDC1负责CD8+ T细胞扩增,反过来,T细胞衍生的IFN-γ增强了cDC1的存活。然而,Flt3L和CD40激动作用通过激活cDC2s增加调节性T细胞,抑制免疫。这些发现支持进一步探索以dc为中心的方法来增强PDAC的抗肿瘤免疫。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Science Immunology
Immunology and Microbiology-Immunology
CiteScore
32.90
自引率
2.00%
发文量
183
期刊介绍:
Science Immunology is a peer-reviewed journal that publishes original research articles in the field of immunology. The journal encourages the submission of research findings from all areas of immunology, including studies on innate and adaptive immunity, immune cell development and differentiation, immunogenomics, systems immunology, structural immunology, antigen presentation, immunometabolism, and mucosal immunology. Additionally, the journal covers research on immune contributions to health and disease, such as host defense, inflammation, cancer immunology, autoimmunity, allergy, transplantation, and immunodeficiency. Science Immunology maintains the same high-quality standard as other journals in the Science family and aims to facilitate understanding of the immune system by showcasing innovative advances in immunology research from all organisms and model systems, including humans.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


