Home video clips compared to polygraphy for obstructive sleep apnea diagnosis in children with autism spectrum disorder: A pilot study
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
Abstract
Introduction
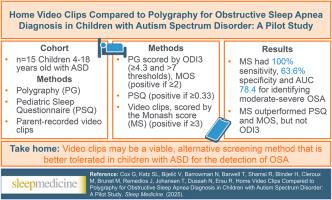
Children with autism spectrum disorder (ASD) have higher prevalence of obstructive sleep apnea (OSA) than typically developing children. Polysomnography (PSG), the gold standard test is challenging for children with ASD. Polygraphy (PG) may be better tolerated, but more accessible screening tools are needed. We evaluated diagnostic characteristics of video clips for OSA in this pilot study.
Methods
Children 4–18 years with ASD referred for PSG for suspected OSA were recruited. Parents recorded 3 2-min home videos, scored for OSA presence using Monash score (MS, positive if ≥ 3). Participants completed the Pediatric Sleep Questionnaire (PSQ; positive if ≥ 0.33) and underwent home PG, scored by obstructive apnea hypopnea index (oAHI), oxygen desaturation index 3 % (ODI3; ≥4.3 and > 7 thresholds) and McGill Oximetry Score (MOS; positive if ≥ 2). Receiver-operator curves were used to compare diagnostic performance across tools for moderate-severe OSA (oAHI ≥5 events/hour).
Results
26 children participated; 15 (median age 7.1) provided video clips. Median oAHI was 2.4/hr; 26.7 % had moderate-severe OSA. Fourteen (93.3 %) had PSQ ≥0.33, three had MOS ≥2. ODI3 was ≥4.3 in 7 and > 7 in 6 children. Median MS was 3.0. MS had 100 % sensitivity, 63.6 % specificity and AUC 78.4 for detecting moderate-severe OSA; average AUC increased when MS was combined with oximetry metrics.
Conclusion
MS showed high sensitivity but low specificity in detecting moderate-severe OSA. MS outperformed PSQ and MOS, but not ODI3. MS may be a viable alternative screening tool to identify OSA in children with ASD but requires further validation.
家庭录像片段与测谎法在自闭症谱系障碍儿童阻塞性睡眠呼吸暂停诊断中的比较:一项初步研究
患有自闭症谱系障碍(ASD)的儿童比正常发育的儿童有更高的阻塞性睡眠呼吸暂停(OSA)患病率。多导睡眠描记仪(PSG)是ASD儿童的黄金标准测试,具有挑战性。测谎仪(PG)可能更容易被接受,但需要更容易获得的筛查工具。在这项初步研究中,我们评估了视频片段对OSA的诊断特征。方法招募4-18岁的ASD患儿,疑似OSA患者行PSG检查。家长录制了3段2分钟的家庭视频,使用莫纳什评分(MS,≥3为阳性)对OSA的存在进行评分。参与者完成了儿童睡眠问卷(PSQ);≥0.33则为阳性),并进行了家庭PG,以阻塞性呼吸暂停低通气指数(oAHI)、氧去饱和指数3% (ODI3;≥4.3和>;7个阈值)和McGill氧饱和度评分(MOS;≥2则为正。采用接受者-操作者曲线比较各种工具对中重度OSA (oAHI≥5事件/小时)的诊断效果。结果26名儿童参与;15名(中位年龄7.1)提供视频剪辑。oAHI中位数为2.4/小时;26.7%为中重度OSA。PSQ≥0.33者14例(93.3%),MOS≥2者3例。ODI3≥4.3在7和>;6个孩子中有7个。中位MS为3.0。MS检测中重度OSA的灵敏度为100%,特异性为63.6%,AUC为78.4;MS联合血氧测定时平均AUC升高。结论ms检测中重度OSA灵敏度高,特异性低。MS优于PSQ和MOS,但不优于ODI3。MS可能是鉴别ASD患儿OSA的一种可行的替代筛查工具,但需要进一步验证。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


