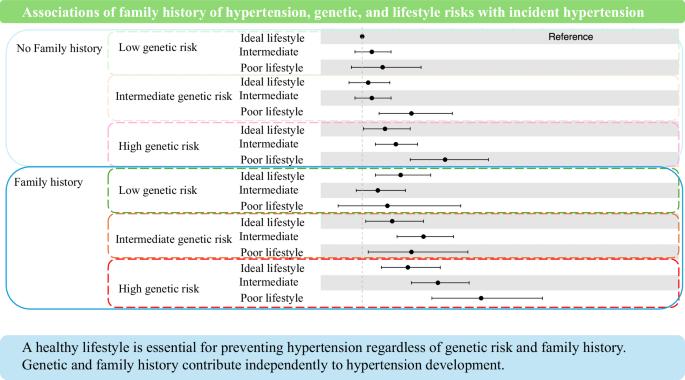
Associations of family history of hypertension, genetic, and lifestyle risks with incident hypertension
IF 4.6
2区 医学
Q1 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
Family history of hypertension may reflect genetic and lifestyle factors. Genetic risk can be assessed using polygenic risk score (PRS); however, whether PRS can stratify hypertension risk when combined with family history and lifestyle information is unclear. This prospective cohort study included 9,001 hypertension-free individuals aged ≥20 years from the Tohoku Medical Megabank Community-Based Cohort Study. Participants were scored on lifestyle factors, including body mass index, urinary sodium-to-potassium ratio, physical activity, alcohol consumption, and smoking at recruitment. During the mean follow-up of 4.3 years, 2822 (31.4%) cases of hypertension occurred. High genetic risk and poor lifestyle were associated with increased hypertension risk. Compared with participants with low genetic risk, ideal lifestyle, and no family history, high genetic risk significantly increased hypertension risk, even among those with ideal lifestyle and no family history (relative risk [RR] 1.28 [95% confidence interval [CI] 1.11–1.46]). Participants with low PRS, ideal lifestyle, but with family history had increased hypertension risk (RR 1.32 [95%CI 1.11–1.57]). Poor lifestyle increased hypertension risk across most genetic risk groups, regardless of family history. Integrating PRS into models with family history and lifestyle risk significantly improved predictive accuracy (area under the curve: 0.671 for family history and lifestyle risk and 0.674 for PRS integrated; P for difference <0.05). Integrating PRS with lifestyle and family history enhances the stratification of individuals at high risk for hypertension.
高血压家族史、遗传和生活方式风险与高血压事件的关系
高血压家族史可能反映遗传和生活方式因素。遗传风险可采用多基因风险评分(PRS)进行评估;然而,当结合家族史和生活方式信息时,PRS是否可以对高血压风险进行分层尚不清楚。这项前瞻性队列研究纳入了9,001名年龄≥20岁的无高血压个体,这些个体来自Tohoku Medical Megabank社区队列研究。研究人员对参与者的生活方式因素进行评分,包括体重指数、尿钠钾比、体力活动、饮酒和吸烟。平均随访4.3年,发生高血压2822例(31.4%)。高遗传风险和不良生活方式与高血压风险增加有关。与低遗传风险、理想生活方式、无家族史的参与者相比,高遗传风险显著增加高血压风险,即使在理想生活方式、无家族史的参与者中也是如此(相对危险度[RR] 1.28[95%置信区间[CI] 1.11-1.46])。低PRS,理想生活方式,但有家族史的参与者高血压风险增加(RR 1.32 [95%CI 1.11-1.57])。无论家族史如何,不良的生活方式增加了大多数遗传风险人群患高血压的风险。将PRS整合到具有家族史和生活方式风险的模型中显著提高了预测精度(曲线下面积:家族史和生活方式风险的曲线下面积为0.671,PRS整合后的曲线下面积为0.674;P代表差分
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Hypertension Research
医学-外周血管病
CiteScore
7.40
自引率
16.70%
发文量
249
审稿时长
3-8 weeks
期刊介绍:
Hypertension Research is the official publication of the Japanese Society of Hypertension. The journal publishes papers reporting original clinical and experimental research that contribute to the advancement of knowledge in the field of hypertension and related cardiovascular diseases. The journal publishes Review Articles, Articles, Correspondence and Comments.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


