The impact of chronic kidney disease on the antithrombotic strategies and outcomes in patients with acute coronary syndromes and atrial fibrillation: Insights from STAR-ACS study
IF 2.1
Q3 PERIPHERAL VASCULAR DISEASE
International Journal of Cardiology Cardiovascular Risk and Prevention
Pub Date : 2025-08-05
DOI:10.1016/j.ijcrp.2025.200486
引用次数: 0
Abstract
Background
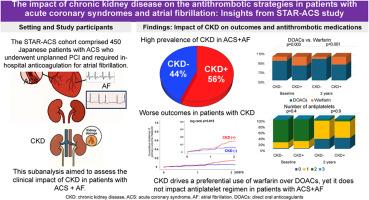
Patients with acute coronary syndrome (ACS) and atrial fibrillation (AF) (ACS + AF) face elevated risks of thrombotic and bleeding events, especially with comorbid chronic kidney disease (CKD). Limited research has assessed the combined influence of CKD in this high-risk population.
Methods
This first subanalysis of STAR-ACS study included 445 Japanese ACS + AF patients, stratified by CKD status (eGFR < vs. ≥ 60 mL/min/1.73 m2, CKD (+) vs. (−) groups, respectively). Antithrombotic therapy was assessed at baseline, one year, and two years. Primary outcomes included major bleeding and major adverse cardiovascular events.
Results
CKD prevalence was high at 56.4 %. While ratio of dual antiplatelet therapy had drastically decreased by two years, there was no significant difference between CKD (+) and (−) groups. In contrast, among anticoagulants, warfarin was preferably used in CKD (+) group, compared to CKD (−) group, remaining stable for 2 years. Direct oral anticoagulants (DOACs) were prescribed less frequently in CKD patients, with rivaroxaban usage notably lower in CKD (+), while apixaban usage numerically increased in CKD patients. Moreover, CKD was associated with a higher cumulative incidence of adverse outcomes, although this was not statistically significant. However, in DOACs-treated patients, CKD was significantly linked to poorer outcomes, with higher eGFR levels correlating with reduced risk.
Conclusions
This real-world data of ACS + AF patients indicated the significant influence of CKD on anticoagulant choice and on the worse outcome trends. These findings highlight the need for tailored antithrombotic strategies in patients with ACS, AF, and CKD to mitigate bleeding and thrombotic risks.
慢性肾脏疾病对急性冠状动脉综合征和心房颤动患者抗血栓策略和结果的影响:来自STAR-ACS研究的见解
背景:急性冠脉综合征(ACS)和心房颤动(AF) (ACS + AF)患者面临血栓形成和出血事件的高风险,特别是合并慢性肾脏疾病(CKD)。有限的研究评估了CKD对这一高危人群的综合影响。方法STAR-ACS研究的第一个亚分析包括445名日本ACS + AF患者,按CKD状态(eGFR和lt;与≥60毫升/分钟/ 1.73平方米,CKD(+)和(−)组,分别)。抗血栓治疗在基线、1年和2年进行评估。主要结局包括主要出血和主要不良心血管事件。结果sckd患病率为56.4%。虽然双重抗血小板治疗的比例在两年内急剧下降,但CKD(+)组和(-)组之间没有显著差异。相比之下,在抗凝剂中,与CKD(−)组相比,CKD(+)组优先使用华法林,保持稳定2年。直接口服抗凝剂(DOACs)在CKD患者中的使用频率较低,利伐沙班在CKD患者中的使用明显较低(+),而阿哌沙班在CKD患者中的使用数量增加。此外,CKD与较高的不良结局累积发生率相关,尽管这没有统计学意义。然而,在doacs治疗的患者中,CKD与较差的预后显著相关,eGFR水平较高与风险降低相关。结论ACS + AF患者的真实数据表明,CKD对抗凝剂选择和不良结局趋势有显著影响。这些发现强调了ACS、AF和CKD患者需要量身定制的抗血栓策略,以减轻出血和血栓风险。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

International Journal of Cardiology Cardiovascular Risk and Prevention
Cardiology and Cardiovascular Medicine
CiteScore
3.00
自引率
0.00%
发文量
0
审稿时长
72 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


