Longitudinal investigation of sleep and circadian rest-activity rhythms in non-small cell lung cancer patients during immunotherapy and associations with fatigue, depression, and perceived stress
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
Abstract
Background
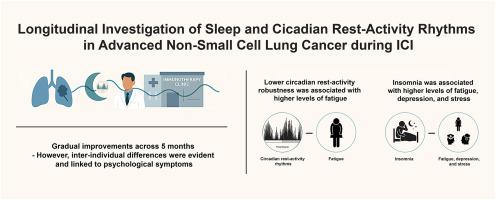
Patients with advanced non-small cell lung cancer (NSCLC) face poor prognosis. However, new therapies like immune checkpoint inhibitors (ICIs) have improved survival. Nevertheless, ICIs act through immune activation – a proposed underlying mechanism of frequently reported symptoms such as sleep and circadian disturbances. The objective of this study was to longitudinally investigate sleep and circadian rest-activity rhythms and associations with psychological symptoms in NSCLC during ICI treatment.
Methods
Newly diagnosed NSCLC patients were included in this prospective study, assessing insomnia severity, total sleep time, circadian rest-activity rhythms, and psychological symptoms (fatigue, depression, and stress) during the first five months of ICI treatment, using validated questionnaires, sleep diaries and actigraphy.
Results
Forty-nine patients were included. Prior to treatment, patients slept on average 5.8 hours/night and 49 % reported clinical levels of insomnia. Spontaneous improvements in insomnia severity and total sleep time were observed, along with marginal but non-significant improvements in circadian rest-activity rhythm robustness. Insomnia severity was significantly associated with higher levels of fatigue (p = .004), depression (p = .007), and perceived stress (p = .033). Moreover, lower circadian rest-activity robustness was associated with more fatigue (p = .021). At baseline, mean levels of fatigue, depression, and perceived stress were below clinical levels and declined further over time.
Conclusion
Sleep disturbances, circadian disruption, and psychological symptom burden in NSCLC patients were greatest prior to and shortly after initiation of ICI treatment, with gradual improvement over the first five months. However, inter-individual differences in sleep and circadian disturbances were evident and linked to psychological symptoms.
免疫治疗期间非小细胞肺癌患者睡眠和昼夜休息活动节律的纵向研究及其与疲劳、抑郁和感知压力的关系
晚期非小细胞肺癌(NSCLC)患者预后较差。然而,像免疫检查点抑制剂(ICIs)这样的新疗法提高了生存率。然而,ICIs通过免疫激活起作用,这是一种经常报道的症状(如睡眠和昼夜节律紊乱)的潜在机制。本研究的目的是纵向调查非小细胞肺癌在ICI治疗期间的睡眠和昼夜休息-活动节律及其与心理症状的关系。方法将新诊断的NSCLC患者纳入本前瞻性研究,使用有效问卷、睡眠日记和活动记录仪评估ICI治疗前5个月的失眠严重程度、总睡眠时间、昼夜休息-活动节律和心理症状(疲劳、抑郁和压力)。结果纳入49例患者。治疗前,患者平均每晚睡眠5.8小时,49%的患者报告失眠的临床水平。观察到失眠严重程度和总睡眠时间的自发改善,以及昼夜休息-活动节律稳健性的边际但不显著的改善。失眠严重程度与较高水平的疲劳(p = 0.004)、抑郁(p = 0.007)和感知压力(p = 0.033)显著相关。此外,较低的昼夜休息活动稳健性与更多的疲劳相关(p = 0.021)。在基线时,疲劳、抑郁和感知压力的平均水平低于临床水平,并随着时间的推移进一步下降。结论:非小细胞肺癌患者的睡眠障碍、昼夜节律紊乱和心理症状负担在ICI治疗开始前和开始后不久最为严重,在前5个月逐渐改善。然而,睡眠和昼夜节律紊乱的个体间差异是明显的,并且与心理症状有关。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


