Social jetlag and obstructive sleep apnea severity: A retrospective study based on polysomnography
IF 3.4
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
Abstract
Background
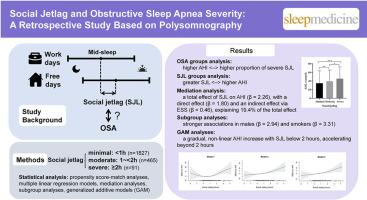
Social jetlag, representing the misalignment between endogenous circadian rhythms and socially imposed sleep schedules, has been associated with various adverse health outcomes. However, its potential relationship with obstructive sleep apnea (OSA) severity, as quantified by the apnea-hypopnea index (AHI), remains unclear.
Methods
This retrospective study analyzed data from participants with OSA (AHI ≥5 events/hour) who completed sleep questionnaires and underwent polysomnography at our sleep center. Exclusions included non-OSA, prior OSA treatment, shift work, sleep-affecting medication use, or incomplete data. Social jetlag was defined as the actual difference between mid-sleep on work days and free days, and categorized as minimal (<1 h), moderate (1 to <2 h), and severe (≥2 h). Multiple linear regression assessed the association between social jetlag and AHI, adjusting for age, gender, body mass index (BMI), history of smoking and alcohol, hypertension, hyperlipidemia, and diabetes. Mediation analysis evaluated the Epworth Sleepiness Scale (ESS) as a mediator, with subgroup analyses and generalized additive models (GAM) exploring effect modification and non-linearity.
Results
Among 2383 analyzed participants, severe social jetlag was independently associated with higher AHI (β = 6.90; 95 % CI: 2.18 to 11.61; p = 0.004; p-trend = 0.014), unlike the moderate group (p = 0.389). ESS mediated 19.4 % of this effect (indirect effect β = 0.46; 95 % CI: 0.22 to 0.72; p < 0.001). In a matched cohort analysis stratified by social jetlag severity (n = 637), AHI and ESS rose with social jetlag severity (AHI: 34.9 vs. 39.4 vs. 45.5 events/hour, p < 0.001; ESS: 10.1 vs. 11.2 vs. 11.8, p = 0.015), while habitual sleep duration decreased (7.0 vs. 6.8 vs. 6.6 h; p = 0.013). Stronger associations were observed in males (β = 2.94; 95 % CI: 1.34 to 4.54; p < 0.001; p-interaction <0.001) and smokers (β = 3.31; 95 % CI: 0.90 to 5.71; p = 0.007; p-interaction = 0.003), with significant effects in BMI 24–28 kg/m2, non-hypertensive, and non-diabetic subgroups (all p < 0.05). GAM analysis revealed a gradual, non-linear AHI increase with social jetlag below 2 h, accelerating beyond 2 h.
Conclusions
Severe Social jetlag independently increases AHI in individuals with OSA, partially mediated by daytime sleepiness, with pronounced effects in males and smokers. These findings suggest circadian misalignment as a potentially modifiable factor influencing OSA severity.
社交时差与阻塞性睡眠呼吸暂停严重程度:一项基于多导睡眠图的回顾性研究
社会时差代表了内源性昼夜节律和社会强加的睡眠时间表之间的不一致,与各种不良健康结果有关。然而,其与阻塞性睡眠呼吸暂停(OSA)严重程度的潜在关系(通过呼吸暂停-低通气指数(AHI)量化)仍不清楚。方法回顾性分析在睡眠中心完成睡眠问卷并接受多导睡眠仪检查的OSA (AHI≥5事件/小时)患者的数据。排除包括非OSA、既往OSA治疗、轮班工作、影响睡眠的药物使用或数据不完整。社会时差被定义为工作日和休息日睡眠中期的实际差异,并分为轻微(1小时)、中度(1至2小时)和严重(≥2小时)。多元线性回归评估了社交时差和AHI之间的关系,调整了年龄、性别、体重指数(BMI)、吸烟和酒精史、高血压、高脂血症和糖尿病。中介分析评估Epworth嗜睡量表(ESS)作为中介,采用亚组分析和广义加性模型(GAM)探索效果的修改和非线性。结果在分析的2383名参与者中,严重的社会时差与较高的AHI独立相关(β = 6.90;95% CI: 2.18 ~ 11.61;p = 0.004;p趋势= 0.014),与中度组不同(p = 0.389)。ESS介导了19.4%的效应(间接效应β = 0.46;95% CI: 0.22 ~ 0.72;p & lt;0.001)。在按社会时差严重程度分层的匹配队列分析中(n = 637), AHI和ESS随社会时差严重程度而上升(AHI: 34.9 vs 39.4 vs 45.5事件/小时,p <;0.001;ESS: 10.1 vs. 11.2 vs. 11.8, p = 0.015),而习惯性睡眠时间减少(7.0 vs. 6.8 vs. 6.6 h;p = 0.013)。在男性中观察到更强的相关性(β = 2.94;95% CI: 1.34 ~ 4.54;p & lt;0.001;p-相互作用<;0.001)和吸烟者(β = 3.31;95% CI: 0.90 ~ 5.71;p = 0.007;p相互作用= 0.003),对BMI 24-28 kg/m2、非高血压和非糖尿病亚组有显著影响(均p <;0.05)。GAM分析显示,在社交时差低于2小时时,AHI呈逐渐、非线性上升,超过2小时后则加速上升。结论严重的社交时差独立增加OSA患者的AHI,部分由白天嗜睡介导,对男性和吸烟者影响明显。这些发现表明,昼夜节律失调是影响OSA严重程度的潜在可改变因素。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


