Effect of Pharmacological Treatment on Exercise-Induced Bronchoconstriction and Allergic Inflammatory Response in Endurance Athletes.
IF 2.1
Q3 SPORT SCIENCES
Ronaldo Aparecido da Silva, Renata Nakata Teixeira, Gerson Dos Santos Leite, Rosana C Agondi, Renata Gorjão, Cristina Maria Kokron, Yara Nely Fiks, Celso Ricardo Fernandes Carvalho
下载PDF
{"title":"Effect of Pharmacological Treatment on Exercise-Induced Bronchoconstriction and Allergic Inflammatory Response in Endurance Athletes.","authors":"Ronaldo Aparecido da Silva, Renata Nakata Teixeira, Gerson Dos Santos Leite, Rosana C Agondi, Renata Gorjão, Cristina Maria Kokron, Yara Nely Fiks, Celso Ricardo Fernandes Carvalho","doi":"10.26603/001c.141859","DOIUrl":null,"url":null,"abstract":"<p><strong>Background: </strong>Endurance athletes (EA) with lung disease and allergic inflammation have worse performance.</p><p><strong>Purpose: </strong>To examine whether pharmacological treatment can reduce airway disorders such as exercise-induced bronchoconstriction (EIB) and allergic inflammatory response (AIR) in EA.</p><p><strong>Study design: </strong>Prospective, controlled clinical trial.</p><p><strong>Methods: </strong>EA who were marathon runners underwent eucapnic voluntary hyperventilation (EVH) for screening assessment. EA who fulfilled the criteria for an EIB+ after an EVH were included in the treatment group (EIB+; n=13), and those who did not were included in the control group (CON; n=18). The athletes were assessed before and 30 days after the intervention. Outcomes included cardiopulmonary exercise testing, lung function, allergic symptoms (allergic questionnaire for athletes [AQUA©]), AIR (T helper [Th]-1, Th2, and Th17 lymphocytes in cell cultures), inflammatory mediator expression, salivary immunoglobulin (Ig)A, blood cortisol, blood IgE levels, and airway inflammation (fraction exhaled nitric oxide [FeNO]). Both groups were advised to keep the same training routine, and only the EIB+ received pharmacological treatment with inhaled corticosteroids (400-800 mcg/day) and long-acting bronchodilators (12 mcg/day). The CON and EIB+ groups underwent the same assessments after the intervention and were compared pre- and post-intervention, and effect sizes were calculated.</p><p><strong>Results: </strong>EIB+ (males, age 28.1±7.4 years, BMI 20.3±1.0 kg/m2) CON (males, age 29.8±6.5 years, BMI 20.5±1.6 kg/m2) participated. At baseline, the O2 peak, lung function, allergic symptoms, IgE, IgA, FeNO levels, and AIR were not significancly different between groups (p>0.05). After pharmacological treatment, only the EIB+ group showed a decrease in EIB (p<0.001) and an increase in VO2peak compared to baseline (p<0.05). However, no difference was observed in the expression of inflammatory mediators (p>0.05).</p><p><strong>Conclusion: </strong>Pharmacological treatment reduces EIB and increases the aerobic perforance/fitness in endurance athletes. These benefits occur without modification of the AIR.</p><p><strong>Level of evidence: </strong>Level II- Prospective Comparative Study.</p>","PeriodicalId":47892,"journal":{"name":"International Journal of Sports Physical Therapy","volume":"20 8","pages":"1222-1231"},"PeriodicalIF":2.1000,"publicationDate":"2025-08-01","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12317798/pdf/","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"International Journal of Sports Physical Therapy","FirstCategoryId":"1085","ListUrlMain":"https://doi.org/10.26603/001c.141859","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"2025/1/1 0:00:00","PubModel":"eCollection","JCR":"Q3","JCRName":"SPORT SCIENCES","Score":null,"Total":0}
引用次数: 0
引用
批量引用
Abstract
Background: Endurance athletes (EA) with lung disease and allergic inflammation have worse performance.
Purpose: To examine whether pharmacological treatment can reduce airway disorders such as exercise-induced bronchoconstriction (EIB) and allergic inflammatory response (AIR) in EA.
Study design: Prospective, controlled clinical trial.
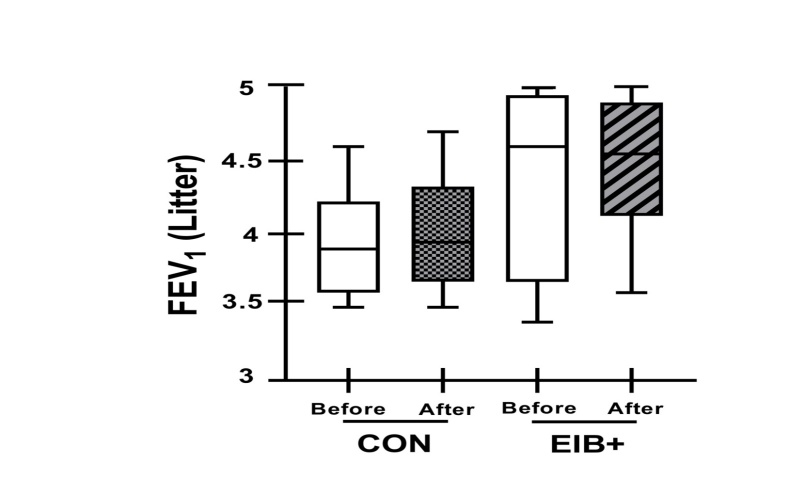
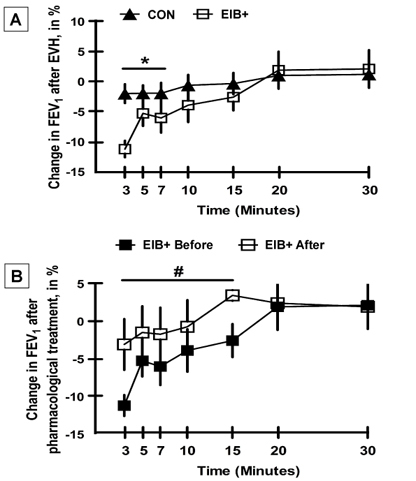
Methods: EA who were marathon runners underwent eucapnic voluntary hyperventilation (EVH) for screening assessment. EA who fulfilled the criteria for an EIB+ after an EVH were included in the treatment group (EIB+; n=13), and those who did not were included in the control group (CON; n=18). The athletes were assessed before and 30 days after the intervention. Outcomes included cardiopulmonary exercise testing, lung function, allergic symptoms (allergic questionnaire for athletes [AQUA©]), AIR (T helper [Th]-1, Th2, and Th17 lymphocytes in cell cultures), inflammatory mediator expression, salivary immunoglobulin (Ig)A, blood cortisol, blood IgE levels, and airway inflammation (fraction exhaled nitric oxide [FeNO]). Both groups were advised to keep the same training routine, and only the EIB+ received pharmacological treatment with inhaled corticosteroids (400-800 mcg/day) and long-acting bronchodilators (12 mcg/day). The CON and EIB+ groups underwent the same assessments after the intervention and were compared pre- and post-intervention, and effect sizes were calculated.
Results: EIB+ (males, age 28.1±7.4 years, BMI 20.3±1.0 kg/m2) CON (males, age 29.8±6.5 years, BMI 20.5±1.6 kg/m2) participated. At baseline, the O2 peak, lung function, allergic symptoms, IgE, IgA, FeNO levels, and AIR were not significancly different between groups (p>0.05). After pharmacological treatment, only the EIB+ group showed a decrease in EIB (p<0.001) and an increase in VO2peak compared to baseline (p<0.05). However, no difference was observed in the expression of inflammatory mediators (p>0.05).
Conclusion: Pharmacological treatment reduces EIB and increases the aerobic perforance/fitness in endurance athletes. These benefits occur without modification of the AIR.
Level of evidence: Level II- Prospective Comparative Study.
药物治疗对耐力运动员运动性支气管收缩和过敏性炎症反应的影响。
背景:患有肺部疾病和过敏性炎症的耐力运动员(EA)表现较差。目的:探讨药物治疗是否能减少运动性支气管收缩(EIB)和过敏性炎症反应(AIR)等气道疾病。研究设计:前瞻性、对照临床试验。方法:对参加马拉松比赛的EA患者进行自发性超换气(EVH)筛查评估。EVH后符合EIB+标准的EA被纳入治疗组(EIB+;n=13),未纳入对照组(CON;n = 18)。在干预前和干预后30天对运动员进行评估。结果包括心肺运动试验、肺功能、过敏症状(运动员过敏问卷[AQUA©])、AIR(细胞培养中辅助性T [Th]-1、Th2和Th17淋巴细胞)、炎症介质表达、唾液免疫球蛋白(Ig)A、血液皮质醇、血液IgE水平和气道炎症(呼出一氧化氮分数[FeNO])。建议两组保持相同的训练常规,只有EIB+组接受吸入皮质类固醇(400-800微克/天)和长效支气管扩张剂(12微克/天)的药物治疗。CON组和EIB+组在干预后进行相同的评估,并比较干预前和干预后的效果,并计算效应量。结果:参加EIB+(男性,年龄28.1±7.4岁,BMI 20.3±1.0 kg/m2) CON(男性,年龄29.8±6.5岁,BMI 20.5±1.6 kg/m2)。基线时,两组患者的O2峰值、肺功能、过敏症状、IgE、IgA、FeNO水平、AIR均无显著差异(p < 0.05)。药物治疗后,只有EIB+组EIB降低(p0.05)。结论:药物治疗可降低耐力运动员的EIB,提高有氧运动能力。这些好处无需修改AIR即可实现。证据等级:二级——前瞻性比较研究。
本文章由计算机程序翻译,如有差异,请以英文原文为准。

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


