Japanese Patients’ Perceptions of Shared Decision-Making in Renal Replacement Therapy
IF 5.7
2区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
Abstract
Introduction
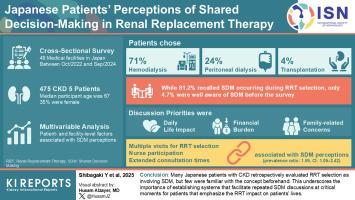
Shared decision-making (SDM) is a key process in selecting renal replacement therapy (RRT). This study analyzed SDM perceptions, preferences, as well as patient- and facility-level factors influencing SDM perception among Japanese patients with chronic kidney disease (CKD) who selected RRT.
Methods
We conducted a cross-sectional survey of 475 adult patients with CKD from 49 medical facilities. SDM awareness and recognition, preferences for SDM timing and frequency, discussion content, and desired professional involvement were assessed. Patient- and facility-level factors associated with SDM perceptions were evaluated using multivariable analysis.
Results
The mean participant age was 67.4 years. Hemodialysis, peritoneal dialysis, and kidney transplantation were chosen by 71%, 24.4%, and 4.4% of patients, respectively. Although 81.2% recalled SDM occurring during RRT selection, only 4.7% were well aware of SDM before the survey. Patients prioritized discussions about daily life impact, financial burden, and family-related concerns. Most patients preferred SDM initiation when RRT was imminent, and to be conducted over multiple sessions. Many patients valued the involvement of medical social workers and their usual nonnephrologist physicians in addition to nephrologists. Multiple outpatient visits for RRT selection, involving nurse participation and extended consultation times, were significantly associated with SDM perceptions (prevalence ratio [PR]: 1.59, 95% confidence interval [CI]: 1.05–2.42).
Conclusion
Many Japanese patients with CKD retrospectively evaluated RRT selection as involving SDM; however, a few were familiar with the concept beforehand. This underscores the importance of establishing systems that facilitate repeated SDM discussions at critical moments for patients. These discussions should emphasize the impact of RRT on patients’ lives and involve a multidisciplinary team.
日本患者对肾脏替代治疗中共同决策的看法
共同决策(SDM)是选择肾脏替代治疗(RRT)的关键过程。本研究分析了选择RRT的日本慢性肾脏疾病(CKD)患者对SDM的感知、偏好以及患者和设施层面的因素对SDM感知的影响。方法我们对来自49家医疗机构的475名成年CKD患者进行了横断面调查。对SDM的认识和认可、对SDM时间和频率的偏好、讨论内容和期望的专业参与进行了评估。使用多变量分析评估与SDM感知相关的患者和设施水平因素。结果平均年龄为67.4岁。选择血液透析、腹膜透析和肾移植的患者分别占71%、24.4%和4.4%。尽管81.2%的人回忆起在RRT选择过程中发生的SDM,但只有4.7%的人在调查前了解SDM。患者优先讨论日常生活影响、经济负担和家庭相关问题。大多数患者倾向于在RRT迫在眉睫时启动SDM,并在多个疗程中进行。许多患者重视医务社会工作者的参与,除了肾病学家之外,他们通常的非肾病学家医生也参与其中。选择RRT的多次门诊就诊,包括护士参与和延长的会诊时间,与SDM感知显著相关(患病率比[PR]: 1.59, 95%置信区间[CI]: 1.05-2.42)。结论许多日本CKD患者回顾性评估RRT选择是否涉及SDM;然而,只有少数人事先熟悉这个概念。这强调了建立系统的重要性,以便在关键时刻为患者反复讨论SDM。这些讨论应强调RRT对患者生活的影响,并涉及多学科团队。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Kidney International Reports
Medicine-Nephrology
CiteScore
7.70
自引率
3.30%
发文量
1578
审稿时长
8 weeks
期刊介绍:
Kidney International Reports, an official journal of the International Society of Nephrology, is a peer-reviewed, open access journal devoted to the publication of leading research and developments related to kidney disease. With the primary aim of contributing to improved care of patients with kidney disease, the journal will publish original clinical and select translational articles and educational content related to the pathogenesis, evaluation and management of acute and chronic kidney disease, end stage renal disease (including transplantation), acid-base, fluid and electrolyte disturbances and hypertension. Of particular interest are submissions related to clinical trials, epidemiology, systematic reviews (including meta-analyses) and outcomes research. The journal will also provide a platform for wider dissemination of national and regional guidelines as well as consensus meeting reports.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


