Attributable burden of steatotic liver disease on cardiovascular outcomes in Asia
IF 7.5
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
Abstract
Background & Aims
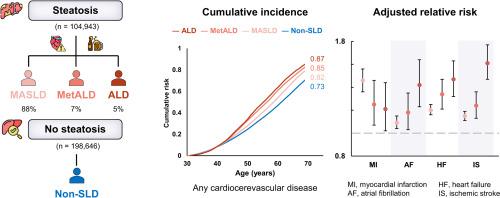
The associations between metabolic dysfunction-associated steatotic liver disease (MASLD) and specific cardiovascular events, as well as their attributable burdens, remain inconsistent and underexplored within a single population. This large-scale prospective cohort evaluated the associations between MASLD and various cardiovascular outcomes. Two additional steatotic liver disease (SLD) subtypes – MASLD with increased alcohol consumption (MetALD) and alcohol-related liver disease (ALD) – were also evaluated.
Methods
We included 303,589 adults aged ≥30 years from Taiwan who underwent health examinations between 1997 and 2013. MASLD was defined by ultrasound-detected steatosis, limited alcohol intake, and ≥1 cardiometabolic risk factor. MetALD and ALD were defined based on alcohol intake thresholds and cardiometabolic profiles. Participants were followed until 2020, with outcomes and mortality ascertained via linkage to national registries. Cox proportional hazards models were used to estimate adjusted relative risks (RRs), and population attributable fractions (PAFs) were calculated.
Results
Of the total population, 91,877 (30.3%) had MASLD, 7,490 (2.5%) had MetALD, 5,576 (1.8%) had ALD, and 198,646 (65.4%) did not have SLD. Over a median follow-up of 10.4 years, 162,959 cardiovascular events occurred. The adjusted RR of any cardiovascular diseases was 1.29 (95% CI 1.38-1.31) for MASLD, 1.38 (95% CI 1.34-1.42) for MetALD, and 1.48 (95% CI 1.43-1.53) for ALD. Among all SLD subtypes, MASLD showed the highest RR for myocardial infarction (RR 1.46, 95% CI 1.36–1.56). Findings remained consistent after accounting for liver-related deaths. The PAF for MASLD was 8.07% (95% CI 7.81–8.58). Despite higher risks, MetALD and ALD had lower PAFs due to lower prevalence.
Conclusions
All major SLD subtypes – MASLD, MetALD, and ALD – were associated with increased long-term cardiovascular risk, underscoring the need for early detection and cardiometabolic risk management across the SLD spectrum.
Impact and implications
This large-scale study of 303,589 individuals demonstrates that metabolic dysfunction-associated steatotic liver disease (MASLD) increases the risk of cardiovascular diseases by at least 29%. Cardiovascular risk further escalates across SLD subtypes with higher levels of alcohol consumption. Notably, MASLD was associated with the highest risk of myocardial infarction among all SLD subtypes. By quantifying population burden, we found that 8.07% of cardiovascular events may be preventable through effective MASLD prevention strategies, highlighting the critical role of cardiometabolic risk management. These findings emphasize the need to integrate MASLD identification and prevention into broader cardiometabolic care and public health frameworks.
Clinical trial number
not applicable.
脂肪变性肝病对亚洲心血管预后的归因负担
背景,目的:在单一人群中,代谢功能障碍相关脂肪变性肝病(MASLD)与特定心血管事件之间的关联及其可归因负担仍不一致且未得到充分探讨。这项大规模前瞻性队列研究评估了MASLD与各种心血管结局之间的关系。另外两种脂肪变性肝病(SLD)亚型——酒精摄入增加的MASLD (MetALD)和酒精相关性肝病(ALD)——也被评估。MASLD的定义是超声检测的脂肪变性、有限的酒精摄入和≥1个心脏代谢危险因素。MetALD和ALD是根据酒精摄入阈值和心脏代谢谱来定义的。参与者被跟踪到2020年,通过与国家登记处的联系确定结果和死亡率。采用Cox比例风险模型估计调整后的相对风险(rr),并计算人群归因分数(paf)。结果MASLD患者91877人(30.3%),MetALD患者7490人(2.5%),ALD患者5576人(1.8%),无SLD患者198646人(65.4%)。在10.4年的中位随访中,发生了162959例心血管事件。MASLD校正后的心血管疾病的RR为1.29 (95% CI 1.38-1.31), MetALD校正后的RR为1.38 (95% CI 1.34-1.42), ALD校正后的RR为1.48 (95% CI 1.43-1.53)。在所有SLD亚型中,MASLD与心肌梗死的RR最高(RR 1.46, 95% CI 1.36-1.56)。考虑到肝脏相关死亡后,研究结果保持一致。MASLD的PAF为8.07% (95% CI 7.81-8.58)。尽管风险较高,但由于患病率较低,MetALD和ALD的paf较低。所有主要的SLD亚型——MASLD、MetALD和ALD——都与长期心血管风险增加相关,强调了SLD谱系早期检测和心脏代谢风险管理的必要性。影响和意义这项涉及303,589人的大规模研究表明,代谢功能障碍相关的脂肪变性肝病(MASLD)使心血管疾病的风险至少增加29%。随着酒精摄入量的增加,心血管风险在SLD亚型中进一步上升。值得注意的是,在所有SLD亚型中,MASLD与心肌梗死的最高风险相关。通过量化人群负担,我们发现通过有效的MASLD预防策略可以预防8.07%的心血管事件,突出了心脏代谢风险管理的关键作用。这些发现强调需要将MASLD的识别和预防纳入更广泛的心脏代谢护理和公共卫生框架。临床试验编号不适用。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

JHEP Reports
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
12.40
自引率
2.40%
发文量
161
审稿时长
36 days
期刊介绍:
JHEP Reports is an open access journal that is affiliated with the European Association for the Study of the Liver (EASL). It serves as a companion journal to the highly respected Journal of Hepatology.
The primary objective of JHEP Reports is to publish original papers and reviews that contribute to the advancement of knowledge in the field of liver diseases. The journal covers a wide range of topics, including basic, translational, and clinical research. It also focuses on global issues in hepatology, with particular emphasis on areas such as clinical trials, novel diagnostics, precision medicine and therapeutics, cancer research, cellular and molecular studies, artificial intelligence, microbiome research, epidemiology, and cutting-edge technologies.
In summary, JHEP Reports is dedicated to promoting scientific discoveries and innovations in liver diseases through the publication of high-quality research papers and reviews covering various aspects of hepatology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


