Association of Abnormal Glucose Metabolism and Inflammation With Prognosis in Patients With Acute Coronary Syndrome
Abstract
Background
In acute coronary syndrome (ACS) patients, the relationship between abnormal glucose metabolism markers, such as the triglyceride-glucose (TyG) index and stress hyperglycemia ratio (SHR), and inflammatory markers remains unclear. Furthermore, their interaction and impact on long-term prognosis have yet to be investigated in clinical cohorts.
Methods
In this study, K-means clustering was performed on the TyG index, SHR, and inflammatory markers, including high mobility group box-1 protein, platelet-derived growth factor, phenylacetylglutamine, lysophosphatidic acid, and citrullinated histone H3. A Cox proportional hazards model was used to assess the association between cluster phenotypes and 1-year major adverse cardiovascular events (MACE) risk in ACS patients.
Results
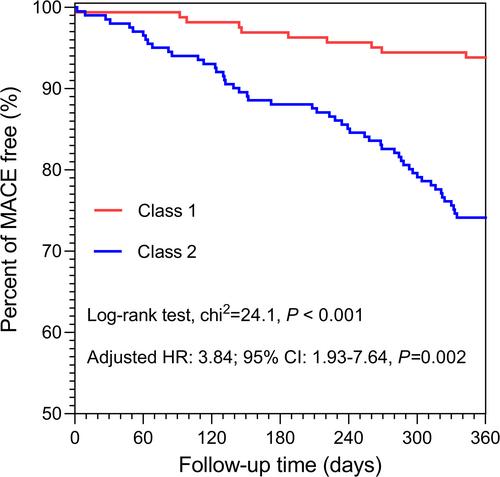
Among 363 ACS patients, 62 developed MACE during the 1-year follow-up. SHR correlated positively with the TyG index and inflammatory markers. K-means clustering identified two phenotypes: normal glucose metabolism/low inflammation and abnormal glucose metabolism/high inflammation. Multivariable Cox analysis showed the latter was strongly linked to MACE (adjusted hazard ratio: 3.84, 95% confidence interval: 1.93–7.64), and early guideline-directed medical therapy reduced MACE risk in this high-risk group.
Conclusions
ACS patients with abnormal glucose metabolism and high inflammation have a higher long-term MACE risk than those with normal glucose metabolism and low inflammation. Early guideline-directed medical therapy, alongside anti-inflammatory therapy and hypoglycemic agents, may improve long-term outcomes in this high-risk group.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


