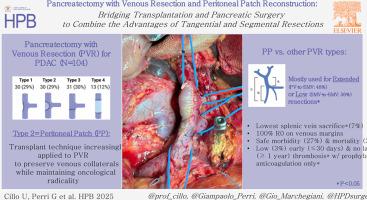
Pancreatectomy with venous resection and peritoneal patch reconstruction: bridging transplantation and pancreatic surgery to combine the advantages of tangential and segmental resections
IF 2.4
3区 医学
Q2 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
Abstract
Background
Pancreatectomy with venous resection (PVR) is considered standard practice and accomplished with different techniques.
Methods
Patients undergoing PVR with portal (PV) and/or superior mesenteric (SMV) vein resection for PDAC between 2015 and 2024 at a high-volume HPB and Liver Transplant Unit were retrospectively analyzed according to ISGPS types.
Results
A total of 104 patients underwent PVR: tangential w/primary closure (Type 1 = 30; 29 %) or peritoneal patch (Type 2 = 30; 29 %), segmental w/primary anastomosis (Type 3 = 31; 30 %) or interposition graft (Type 4 = 13; 12 %). Type 2 was mostly used for low (SMV-to-SMV = 37 %) or extended (PV-to-SMV = 50 %) resections (p < 0.001), with lowest rate of splenic vein sacrifice (7 %; p = 0.001). Major morbidity and hemorrhage (PPH) were similar among different ISGPS types (Type 2 = 27 % and 30 %, respectively), as well as mortality (Type 2 = 3 % at 90 days). Prophylactic dose anticoagulation was used in 73 % of Type 2 patients, with 3 % early (≤30 days) and no late (≤1 year) thrombosis.
Discussion
The peritoneal patch offers the advantages of both tangential and segmental resections. It can be used for low or extended infiltrations, preserving venous collaterals without sacrificing radicality, with acceptable morbidity and mortality, and near-zero thrombotic events using prophylactic anticoagulation only.
胰切除术联合静脉切除和腹膜补片重建:桥接移植和胰手术结合切向和节段切除的优点。
背景:胰切除术与静脉切除术(PVR)被认为是标准的做法,并完成不同的技术。方法:回顾性分析2015 - 2024年在大容量HPB和肝移植单元进行PVR合并门静脉(PV)和/或肠系膜上静脉(SMV)切除术的PDAC患者,并根据ISGPS类型进行分析。结果:共有104例患者接受了PVR:切向闭合/初级闭合(1型= 30;29%)或腹膜贴片(2型= 30;29%),节段性w/一期吻合(3型= 31;30%)或间接性移植物(4型= 13;12%)。2型主要用于低位(SMV-to-SMV = 37%)或扩展(PV-to-SMV = 50%)切除(p < 0.001),脾静脉牺牲率最低(7%;P = 0.001)。不同ISGPS类型的主要发病率和出血(PPH)相似(2型分别为27%和30%),以及死亡率(90天时2型= 3%)。73%的2型患者使用了预防性剂量抗凝,3%的患者早期(≤30天)血栓形成,晚期(≤1年)无血栓形成。讨论:腹膜贴片提供切向和节段切除的优点。它可用于低浸润或扩展浸润,在不牺牲根治性的情况下保留静脉侧支,具有可接受的发病率和死亡率,并且仅使用预防性抗凝治疗几乎零血栓事件。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Hpb
GASTROENTEROLOGY & HEPATOLOGY-SURGERY
CiteScore
5.60
自引率
3.40%
发文量
244
审稿时长
57 days
期刊介绍:
HPB is an international forum for clinical, scientific and educational communication.
Twelve issues a year bring the reader leading articles, expert reviews, original articles, images, editorials, and reader correspondence encompassing all aspects of benign and malignant hepatobiliary disease and its management. HPB features relevant aspects of clinical and translational research and practice.
Specific areas of interest include HPB diseases encountered globally by clinical practitioners in this specialist field of gastrointestinal surgery. The journal addresses the challenges faced in the management of cancer involving the liver, biliary system and pancreas. While surgical oncology represents a large part of HPB practice, submission of manuscripts relating to liver and pancreas transplantation, the treatment of benign conditions such as acute and chronic pancreatitis, and those relating to hepatobiliary infection and inflammation are also welcomed. There will be a focus on developing a multidisciplinary approach to diagnosis and treatment with endoscopic and laparoscopic approaches, radiological interventions and surgical techniques being strongly represented. HPB welcomes submission of manuscripts in all these areas and in scientific focused research that has clear clinical relevance to HPB surgical practice.
HPB aims to help its readers - surgeons, physicians, radiologists and basic scientists - to develop their knowledge and practice. HPB will be of interest to specialists involved in the management of hepatobiliary and pancreatic disease however will also inform those working in related fields.
Abstracted and Indexed in:
MEDLINE®
EMBASE
PubMed
Science Citation Index Expanded
Academic Search (EBSCO)
HPB is owned by the International Hepato-Pancreato-Biliary Association (IHPBA) and is also the official Journal of the American Hepato-Pancreato-Biliary Association (AHPBA), the Asian-Pacific Hepato Pancreatic Biliary Association (A-PHPBA) and the European-African Hepato-Pancreatic Biliary Association (E-AHPBA).
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


