Factors influencing hepatitis C test uptake following exposure to an infected healthcare worker: Insights from a patient notification exercise
IF 3.2
3区 医学
Q1 PUBLIC, ENVIRONMENTAL & OCCUPATIONAL HEALTH
引用次数: 0
Abstract
Objectives
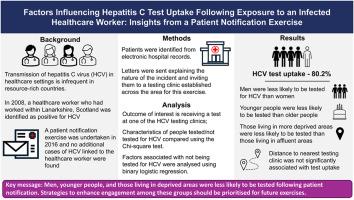
Following the identification of a hepatitis C (HCV) RNA positive healthcare worker, a Patient Notification Exercise (PNE) was undertaken in Lanarkshire, Scotland in 2016. This study analyses the results of the PNE to explore the demographics of those contacted and examines the factors associated, particularly geographic distance to a testing clinic, was associated with not being tested.
Study design
Cross-sectional observational study.
Methods
Eligible patients were identified using electronic health records and offered HCV screening through local clinics. A cross-sectional study examined demographics of the cohort and factors associated with not being tested for HCV were analysed using binary logistic regression.
Results
The study cohort included 6828 individuals, and 19.8 % of these were not tested for HCV during the PNE. In the regression analysis, the odds of not being tested were highest in men (adjusted OR = 1.79, 95 % CI 1.57–2.02, p < 0.0001), those aged <30 years (aOR = 2.76, 95 % CI 1.98–3.85, p < 0.0001) and those living in the most deprived areas (aOR = 1.58, 95 % CI 1.29–1.92, p < 0.001). There was no evidence that distance to testing clinic was a barrier to testing.
Conclusions
The PNE had a high response rate with 80.2 % test uptake and no additional related infections were found Test uptake varied across different groups with men, younger people and those living in deprived areas less likely to participate. Targeted strategies, such as tailored communication or increased testing options, should be used to improve uptake rates in future exercises.
接触受感染医护人员后影响丙型肝炎测试吸收的因素:来自患者通知练习的见解
2016年,在苏格兰拉纳克郡发现一名丙型肝炎(HCV) RNA阳性医护人员后,开展了一次患者通报演习(PNE)。本研究分析了PNE的结果,以探索接触者的人口统计数据,并检查了相关因素,特别是与检测诊所的地理距离,与未接受检测有关。研究设计横断面观察性研究。方法使用电子健康记录识别符合条件的患者,并通过当地诊所进行HCV筛查。横断面研究检查了该队列的人口统计学特征,并使用二元逻辑回归分析了未进行HCV检测的相关因素。结果该研究队列包括6828人,其中19.8%的人在PNE期间未进行HCV检测。在回归分析中,男性未接受检测的几率最高(调整后OR = 1.79, 95% CI 1.57-2.02, p <;0.0001), 30岁患者(aOR = 2.76, 95% CI 1.98-3.85, p <;0.0001)和生活在最贫困地区的人(aOR = 1.58, 95% CI 1.29-1.92, p <;0.001)。没有证据表明距离检测诊所是检测的障碍。结论PNE的有效率为80.2%,未发现额外的相关感染,不同人群的测试吸收率不同,男性,年轻人和生活在贫困地区的人参与测试的可能性较小。应该采用有针对性的策略,如量身定制的沟通或增加测试选项,以提高今后练习中的吸收率。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Public Health
医学-公共卫生、环境卫生与职业卫生
CiteScore
7.60
自引率
0.00%
发文量
280
审稿时长
37 days
期刊介绍:
Public Health is an international, multidisciplinary peer-reviewed journal. It publishes original papers, reviews and short reports on all aspects of the science, philosophy, and practice of public health.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


