Factores asociados a la dehiscencia de anastomosis postoperatoria y comparación de 4 escalas de predicción en cirugía colorrectal
IF 0.8
Q3 ANESTHESIOLOGY
Revista Espanola de Anestesiologia y Reanimacion
Pub Date : 2025-05-10
DOI:10.1016/j.redar.2025.501852
引用次数: 0
Abstract
Introduction
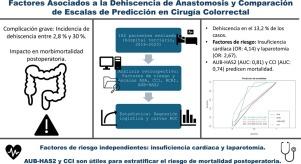
Anastomotic leakage is a serious post-colorectal surgery complication, and has an incidence ranging from 2.8% to 30%. Identifying risk factors and evaluating prediction scores could optimize perioperative management. This study analyses factors associated with dehiscence and compares the predictive capacity of four scales: ASA, CCI, RCRI and AUB-HAS2.
Methods
Retrospective observational study in 182 patients undergoing colorectal surgery with anastomosis in a Spanish tertiary hospital (2018-2020). Clinical and perioperative data were collected, and the ASA, CCI, RCRI and AUB-HAS2 scores were calculated. Risk factors were analysed using multivariate logistic regression, and predictive capacity was assessed with ROC curves.
Results
Leakage occurred in 13.2% of cases. In the multivariate analysis, heart failure (OR: 4.14; 95% CI: 1.14-13.77) and laparotomy (OR: 2.67; 95% CI: 1.07-6.60) were significantly associated with dehiscence. None of the scales predicted this complication. The AUB-HAS2 and CCI scales were associated with 30-day mortality (AUC: 0.81 and 0.74, respectively), and the CCI predicted the need for organ support (AUC: 0.71).
Conclusion
Heart failure and laparotomy are independent risk factors for anastomotic leakage. Although none of the scales predicted this complication, the AUB-HAS2 and CCI were useful in stratifying postoperative mortality. This highlights the importance of personalized assessment.
与术后关节扩张相关的因素和结肠直肠手术4个预测量表的比较
吻合口瘘是结直肠术后严重的并发症,发生率为2.8% ~ 30%。识别危险因素并评价预测评分可优化围手术期管理。本研究分析了崩裂的相关因素,并比较了ASA、CCI、RCRI和AUB-HAS2四种量表的预测能力。方法对2018-2020年西班牙某三级医院182例结直肠吻合术患者进行回顾性观察。收集临床及围手术期资料,计算ASA、CCI、RCRI、AUB-HAS2评分。多因素logistic回归分析危险因素,ROC曲线评估预测能力。结果13.2%的病例发生渗漏。在多变量分析中,心力衰竭(OR: 4.14;95% CI: 1.14-13.77)和剖腹手术(OR: 2.67;95% CI: 1.07-6.60)与裂裂显著相关。所有的量表都没有预测到这种并发症。AUB-HAS2和CCI量表与30天死亡率相关(AUC分别为0.81和0.74),CCI预测器官支持需求(AUC为0.71)。结论心衰和剖腹手术是吻合口瘘的独立危险因素。虽然没有一种量表能预测这种并发症,但AUB-HAS2和CCI对术后死亡率分层是有用的。这突出了个性化评估的重要性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Revista Espanola de Anestesiologia y Reanimacion
ANESTHESIOLOGY-
CiteScore
1.80
自引率
15.40%
发文量
113
审稿时长
82 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


