Reglas de predicción clínica en los pacientes con dolor neuropático periférico de etiología traumática tratados con parche de capsaicina al 8%
IF 0.8
Q3 ANESTHESIOLOGY
Revista Espanola de Anestesiologia y Reanimacion
Pub Date : 2025-06-26
DOI:10.1016/j.redar.2025.501880
引用次数: 0
Abstract
Background and objectives
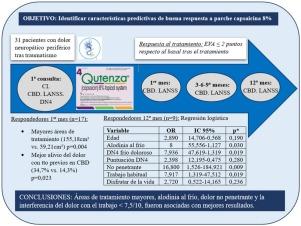
Neuropathic pain (NP) is a widespread, complex disorder that responds differently to pharmacological treatment. The aim of this study was to identify the baseline characteristics of good response to capsaicin 8% patch in patients with trauma-induced peripheral neuropathic pain (PNP).
Materials and methods
We performed a prospective, longitudinal, open-label study in 31 patients with PNP treated with 1-3 applications of the capsaicin 8% patch for 52 weeks. Response to treatment was defined as a reduction in the Visual Analogue Scale (VAS) score compared to baseline. Data from responders and non-responders were compared at the start (month 1) and end (month 12) of treatment. Logistic regression was used to identify predictors of treatment response.
Results
At month 1, responders (n = 17) had significantly larger treatment areas (155.18 cm2 vs. 59.21 cm2; P=.004) and reported greater pain relief with treatments received in the previous week in the brief pain questionnaire (34.7% vs. 14.3%; P=.023). At month 12, significant predictors included cold allodynia (OR 8; P=.030), positive for painful cold in the DN4 questionnaire (OR 7.936; P=.019), no penetrating pain (OR 16.800; P=.009), and pain interference with work score < 7.5 (OR 7.917; P=.019).
Conclusions
This study makes a significant contribution to the management of post-traumatic peripheral neuropathic pain by providing tools to personalize treatment and optimize available resources.
用辣椒素贴片治疗的外源性周围神经性疼痛患者的临床预测规则
背景和目的神经性疼痛(NP)是一种广泛而复杂的疾病,对药物治疗的反应不同。本研究的目的是确定8%辣椒素贴片对创伤性周围神经性疼痛(PNP)患者良好反应的基线特征。材料和方法我们对31例PNP患者进行了一项前瞻性、纵向、开放标签的研究,这些患者接受1-3次8%辣椒素贴剂治疗,持续52周。对治疗的反应被定义为视觉模拟量表(VAS)评分较基线的降低。在治疗开始(第1个月)和结束(第12个月)比较应答者和无应答者的数据。采用Logistic回归来确定治疗反应的预测因素。结果在第1个月,有应答者(n = 17)的治疗面积显著增大(155.18 cm2 vs. 59.21 cm2;P= 0.004),并且在简短疼痛问卷中报告前一周接受治疗的患者疼痛缓解更大(34.7% vs. 14.3%;P = 0)。在第12个月,显著的预测因子包括冷性异常性痛(OR 8;P= 0.030), DN4问卷中疼痛性感冒阳性(OR 7.936;P= 0.019),无穿透性疼痛(OR 16.800;P= 0.009),疼痛干扰工作得分<;7.5(或7.917;P = .019)。结论本研究为创伤后周围神经性疼痛的治疗提供了个性化治疗和优化现有资源的工具,对创伤后周围神经性疼痛的治疗有重要贡献。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Revista Espanola de Anestesiologia y Reanimacion
ANESTHESIOLOGY-
CiteScore
1.80
自引率
15.40%
发文量
113
审稿时长
82 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


