Breast and gynecological cancer risk in systemic lupus erythematosus: A meta-analysis of cohort studies
IF 8.3
1区 医学
Q1 IMMUNOLOGY
引用次数: 0
Abstract
Objective
To evaluate the association between systemic lupus erythematosus (SLE) and the risk of breast and gynecological cancers through a systematic review and meta-analysis of cohort studies.
Methods
A comprehensive search was conducted in PubMed, Embase, and the Cochrane Library. The quality of the studies was assessed using the Newcastle-Ottawa Scale (NOS). Statistical analyses were performed, with separate analyses for standardized incidence ratios (SIRs) and 95 % confidence intervals (CIs). Sensitivity analyses, publication bias assessment using funnel plots and Egger's regression test, and subgroup analyses were conducted.
Results
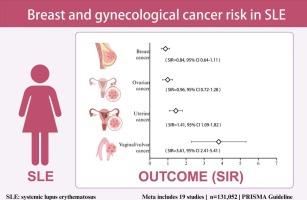
The meta-analysis found no significant association between SLE and risk of breast cancer (SIR = 0.84, 95 % CI 0.64–1.11), I2 = 97.8 %, P = 0.000) or ovarian cancer (SIR = 0.96, 95 % CI 0.72–1.28, I2 = 60.9 %, P = 0.003). However, a significant increase in uterine cancer risk was observed (SIR = 1.41, 95 % CI 1.09–1.82, I2 = 94.3 %, P = 0.000). The strongest association was found for vaginal/vulvar cancer (SIR = 3.61, 95 % CI 2.41–5.41, I2 = 66.6 %, P = 0.006). Subgroup analyses indicated significant regional variations. European patients showed reduced breast cancer risk (SIR = 0.73, 95 % CI 0.57–0.94), while no significant association was observed in Asian or North American populations. Patients from developed countries had lower ovarian cancer risk than those from developing countries (SIR = 0.82, 95 % CI 0.59–1.60).
Conclusion
SLE is associated with an increased risk of uterine and vaginal/vulvar cancers, but not with breast or ovarian cancers. Subgroup analyses reveal regional differences in the relationship between SLE and breast/gynecological cancers.
系统性红斑狼疮的乳腺癌和妇科癌症风险:队列研究的荟萃分析
目的通过对队列研究的系统回顾和荟萃分析,评估系统性红斑狼疮(SLE)与乳腺癌和妇科癌症风险的关系。方法在PubMed、Embase、Cochrane图书馆进行综合检索。研究的质量采用纽卡斯尔-渥太华量表(NOS)进行评估。进行统计分析,分别对标准化发病率(SIRs)和95%置信区间(ci)进行分析。进行敏感性分析、发表偏倚评价(采用漏斗图和Egger’s回归检验)和亚组分析。结果荟萃分析发现SLE与乳腺癌(SIR = 0.84, 95% CI 0.64-1.11), I2 = 97.8%, P = 0.000)或卵巢癌(SIR = 0.96, 95% CI 0.72-1.28, I2 = 60.9%, P = 0.003)风险无显著相关性。然而,子宫癌风险明显增加(SIR = 1.41, 95% CI 1.09-1.82, I2 = 94.3%, P = 0.000)。与阴道/外阴癌相关性最强(SIR = 3.61, 95% CI 2.41 ~ 5.41, I2 = 66.6%, P = 0.006)。亚组分析显示显著的区域差异。欧洲患者乳腺癌风险降低(SIR = 0.73, 95% CI 0.57-0.94),而在亚洲或北美人群中未观察到显著关联。发达国家患者患卵巢癌的风险低于发展中国家患者(SIR = 0.82, 95% CI 0.59-1.60)。结论sle与子宫癌和阴道/外阴癌的风险增加相关,但与乳腺癌或卵巢癌无关。亚组分析显示SLE与乳腺癌/妇科癌症之间的关系存在地区差异。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Autoimmunity reviews
医学-免疫学
CiteScore
24.70
自引率
4.40%
发文量
164
审稿时长
21 days
期刊介绍:
Autoimmunity Reviews is a publication that features up-to-date, structured reviews on various topics in the field of autoimmunity. These reviews are written by renowned experts and include demonstrative illustrations and tables. Each article will have a clear "take-home" message for readers.
The selection of articles is primarily done by the Editors-in-Chief, based on recommendations from the international Editorial Board. The topics covered in the articles span all areas of autoimmunology, aiming to bridge the gap between basic and clinical sciences.
In terms of content, the contributions in basic sciences delve into the pathophysiology and mechanisms of autoimmune disorders, as well as genomics and proteomics. On the other hand, clinical contributions focus on diseases related to autoimmunity, novel therapies, and clinical associations.
Autoimmunity Reviews is internationally recognized, and its articles are indexed and abstracted in prestigious databases such as PubMed/Medline, Science Citation Index Expanded, Biosciences Information Services, and Chemical Abstracts.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


