Dietary risk factors for inflammatory bowel disease: A systematic review and meta-analysis
Q3 Nursing
引用次数: 0
Abstract
Background
Existing evidence indicates that diet is a modifiable risk factor for IBD. However, data on certain nutrients, food groups and individual food items and their associations with IBD is still lacking. This review aims to systematically assess which dietary factors are associated with the onset of IBD.
Method
Computerised bibliographic searches of Ovid MEDLINE, Web of Science, and the Cochrane Library (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Methodology Register) were conducted. Studies were included if they were case-control, cohort studies or randomised controlled trials (RCTs) investigating the association between dietary risk factors and onset of IBD and if they included patients with a diagnosis of IBD (including Crohn's Disease [CD] and/or Ulcerative Colitis [UC]), defined and measured according to clinical symptoms, endoscopy, and histology. Summary relative risks (RRs) were calculated using random effects models to provide risk estimates for the associations between dietary factors and IBD.
Results
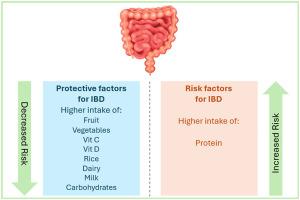
Twenty eligible studies were identified and included in the systematic review and meta-analysis, encompassing 10 case-control and 10 cohort studies, with no RCTs identified. A total of 4,332 patients with IBD were included (1554 CD; 2550 UC; 225 IBD; 3 IBD unclassified [IBDU]). Nine significant predictors of IBD risk were identified. Pooled analysis highlighted a decreased risk of overall IBD was associated with high intakes of fruit (RR 0.70, 95% CI 0.45–0.96), vegetables (RR 0.48, 95% CI 0.19–0.78), carbohydrates (RR 0.70, 95% CI 0.51–0.89), rice (RR 0.65, 95% CI 0.32–0.97), milk (RR 0.43, 95% CI 0.25–0.62), dairy (RR 0.67, 95% CI 0.38–0.97), vitamin C (RR 0.65, 95% CI 0.35–0.96) and vitamin D (RR 0.72, 95% CI 0.46–0.97). High protein intake was associated with a 4.1-fold (RR 4.07, 95% CI 1.51–6.62) increased risk of IBD.
Conclusion
This systematic review and meta-analysis highlights the potential role of diet as a modifiable risk factor for IBD. From a patient management perspective, our results may aid clinicians and dietary practitioners in guiding dietary interventions and modifications, particularly in those at a high-risk of developing the disease. Moreover, our results provide novel data on specific food items and vitamins which may confer a protective effect against IBD, of which evidence has previously been lacking.
炎症性肠病的饮食危险因素:系统回顾和荟萃分析
现有证据表明,饮食是可改变的IBD危险因素。然而,关于某些营养素、食物组和个别食物及其与IBD的关系的数据仍然缺乏。本综述旨在系统地评估哪些饮食因素与IBD的发病有关。方法计算机检索Ovid MEDLINE、Web of Science和Cochrane图书馆(Cochrane系统评价数据库、Cochrane中央对照试验登记册(Central)、Cochrane方法学登记册)的书目。研究纳入病例对照、队列研究或随机对照试验(RCTs),调查饮食危险因素与IBD发病之间的关系,并纳入诊断为IBD(包括克罗恩病[CD]和/或溃疡性结肠炎[UC])的患者,根据临床症状、内窥镜检查和组织学定义和测量。使用随机效应模型计算总结相对风险(rr),以提供饮食因素与IBD之间关联的风险估计。结果20项符合条件的研究被纳入系统评价和荟萃分析,包括10项病例对照研究和10项队列研究,未发现随机对照试验。共有4332例IBD患者被纳入研究(1554例CD;2550年加州大学;225炎症性肠病;3 IBD未分类[IBDU])。确定了IBD风险的9个重要预测因素。综合分析强调,总体IBD风险降低与大量摄入水果(RR 0.70, 95% CI 0.45-0.96)、蔬菜(RR 0.48, 95% CI 0.19-0.78)、碳水化合物(RR 0.70, 95% CI 0.51-0.89)、大米(RR 0.65, 95% CI 0.32-0.97)、牛奶(RR 0.43, 95% CI 0.25-0.62)、乳制品(RR 0.67, 95% CI 0.38-0.97)、维生素C (RR 0.65, 95% CI 0.35-0.96)和维生素D (RR 0.72, 95% CI 0.46-0.97)有关。高蛋白摄入与IBD风险增加4.1倍(RR 4.07, 95% CI 1.51-6.62)相关。结论:本系统综述和荟萃分析强调了饮食作为IBD可改变危险因素的潜在作用。从患者管理的角度来看,我们的研究结果可以帮助临床医生和饮食从业者指导饮食干预和调整,特别是在那些发展为疾病的高风险人群中。此外,我们的研究结果提供了关于特定食物和维生素可能对IBD具有保护作用的新数据,这是以前缺乏的证据。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Clinical Nutrition Open Science
Nursing-Nutrition and Dietetics
CiteScore
2.20
自引率
0.00%
发文量
55
审稿时长
18 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


