Differential Effects of Repetitive Transcranial Magnetic Stimulation on Mood and Pain Symptoms in People With Chronic Pain and Major Depressive Disorders—A Review
Abstract
Background and Objective
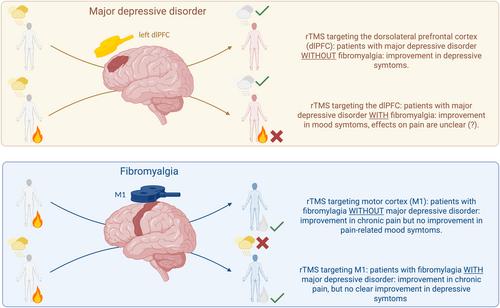
Chronic pain and major depressive disorder (MDD) are among the most prevalent and disabling conditions globally, often co-occurring and sharing overlapping symptoms such as fatigue, cognitive dysfunction and mood disturbances. While fibromyalgia, a primary pain syndrome, and MDD have distinct clinical manifestations, their comorbidity presents therapeutic challenges. Repetitive transcranial magnetic stimulation (rTMS), a non-invasive neuromodulation technique, has shown efficacy in treating both pain and mood disorders when targeted at specific brain regions (motor cortex for pain, dorsolateral prefrontal cortex for mood). This review aimed to investigate whether rTMS interventions for fibromyalgia or MDD improve symptoms across both domains, particularly in comorbid cases.
Databases and Data Treatment
A structured search of PubMed was conducted between January and February 2025. Clinical trials were included if they were randomised, peer-reviewed, in English and involved ≥ 30 participants. Studies included addressed rTMS effects on pain in MDD or mood in fibromyalgia, or both. Out of 143 identified articles, 36 met the inclusion criteria.
Conclusion
Evidence shows rTMS has target- and symptom-specific effects: Motor cortex stimulation improves pain without reliably affecting mood, while dorsolateral prefrontal cortex stimulation alleviates depressive symptoms but inconsistently influences pain. These outcomes suggest that symptom improvement with rTMS is not global over different symptom clusters, but rather different for specific syndromes and the respective neural networks engaged by therapy. Personalised treatment strategies guided by pre-treatment connectivity profiles and symptom clusters, already in use for psychiatric disorders, could enhance outcomes in chronic pain management. However, limitations include small sample sizes, low session numbers and potential floor effects in studies involving non-depressed fibromyalgia patients.
Significance
Noninvasive neuromodulation therapy with repetitive transcranial magnetic stimulation for chronic pain improves pain on fibromyalgia and neuropathic pain but does not improve mood symptoms significantly. Therapy targeting mood symptoms in people with major depressive disorder may have antinociceptive effects in experimental pain models but are not clearly detectable in instances of clinical pain. The relationship between a disease and its associated symptoms is not linear or monotonic and differ between individuals. Unrevealing the associations between individual changes in brain connectivity during disease and the emergence of symptoms is central for the design of personalized and more effective therapeutic interventions.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


