Systemic hypotension and patterns of cerebral blood perfusion in newborns
IF 2.4
3区 医学
Q2 OBSTETRICS & GYNECOLOGY
引用次数: 0
Abstract
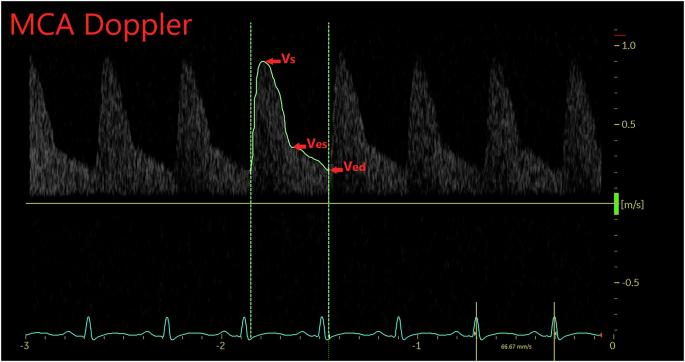
The relationship between systemic hemodynamics and cerebral perfusion in neonates, particularly those with systemic hypotension, is complex and not clearly elucidated. Targeted neonatal echocardiography (TNE) provides valuable insights into cerebral hemodynamics by quantifying middle cerebral artery (MCA) flow in the context of systemic hemodynamics. To investigate the correlation between blood pressure (BP), cardiac output (CO), and MCA Doppler indices in neonates, hypothesizing that BP alone is not a reliable measure of cerebral perfusion. A retrospective cohort study of neonates who underwent their first TNE in the Neonatal Intensive Care Unit. The analysis focused on the relationship between BP components and MCA Doppler measures (i.e., resistive index and pulsatility index). The study included 194 neonates born at a mean gestational age and weight of 30.7 ± 6 weeks and 1744 ± 1246 g, respectively, classified into normotensive, hypotensive, and normotensive-treated groups. Weak correlations were observed between MCA Doppler measures and BP components across the entire cohort. Group comparisons found that neonates in the hypotensive group exhibited higher MCA-RI compared to both normotensive and normotensive-treated groups. Exploratory analyses revealed significant variation in MCA-RI that was explained by cardiac output after accounting for BP and gestational age. These findings suggest that BP alone is not a sufficient indicator of cerebral perfusion status. While the correlations were expected to be weak given the dynamic nature of cardiac output, the results highlight the need for comprehensive hemodynamic assessments in neonates with cardiovascular compromise to avoid reliance on oversimplified metrics such as BP versus Dopplers.
新生儿全身性低血压与脑血流灌注模式。
背景:新生儿全身血流动力学和脑灌注之间的关系是复杂的,而且尚未明确阐明,特别是那些有全身性低血压的新生儿。定向新生儿超声心动图(TNE)通过量化大脑中动脉(MCA)血流,在全身血流动力学的背景下,为大脑血流动力学提供了有价值的见解。目的:探讨新生儿血压(BP)、心输出量(CO)和MCA多普勒指数之间的相关性,假设单独的BP不是脑灌注的可靠指标。方法:对在新生儿重症监护室首次接受TNE的新生儿进行回顾性队列研究。重点分析了血压成分与MCA多普勒测量(即电阻指数和脉搏指数)之间的关系。结果:194例平均胎龄为30.7±6周、体重为1744±1246 g的新生儿分为正常血压组、低血压组和正常血压治疗组。在整个队列中,MCA多普勒测量与BP成分之间观察到弱相关性。组间比较发现,与正常血压组和正常血压组相比,降压药组的新生儿表现出更高的MCA-RI。探索性分析显示,在考虑血压和胎龄后,心输出量可以解释MCA-RI的显著变化。结论:这些发现提示单独的血压不是脑灌注状态的充分指标。虽然考虑到心输出量的动态特性,相关性预计会很弱,但结果强调需要对心血管损害的新生儿进行全面的血液动力学评估,以避免依赖过于简化的指标,如BP与多普勒。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Perinatology
医学-妇产科学
CiteScore
5.40
自引率
6.90%
发文量
284
审稿时长
3-8 weeks
期刊介绍:
The Journal of Perinatology provides members of the perinatal/neonatal healthcare team with original information pertinent to improving maternal/fetal and neonatal care. We publish peer-reviewed clinical research articles, state-of-the art reviews, comments, quality improvement reports, and letters to the editor. Articles published in the Journal of Perinatology embrace the full scope of the specialty, including clinical, professional, political, administrative and educational aspects. The Journal also explores legal and ethical issues, neonatal technology and product development.
The Journal’s audience includes all those that participate in perinatal/neonatal care, including, but not limited to neonatologists, perinatologists, perinatal epidemiologists, pediatricians and pediatric subspecialists, surgeons, neonatal and perinatal nurses, respiratory therapists, pharmacists, social workers, dieticians, speech and hearing experts, other allied health professionals, as well as subspecialists who participate in patient care including radiologists, laboratory medicine and pathologists.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


