ApoB, LDL-C, and non-HDL-C as markers of cardiovascular risk
IF 4.6
3区 医学
Q2 PHARMACOLOGY & PHARMACY
引用次数: 0
Abstract
BACKGROUND
Conventional statistical approaches are not designed to compare highly correlated variables such as low-density lipoprotein cholesterol (LDL-C), non-high density lipoprotein cholesterol (non-HDL-C), and apolipoprotein B (apoB). Discordance analysis was designed to overcome this limitation by creating groups in which the predictions of 2 markers differ.
OBJECTIVE
This systematic review compiled all discordance studies that compare the predictive powers of LDL-C and non-HDL-C vs LDL particle number (LDL P) or apoB as markers of atherosclerotic disease risk to determine which is the most accurate marker of cardiovascular risk.
METHODS
A PubMed search completed September 30, 2024, identified 15 studies involving 593,354 participants. These studies encompassed diverse populations, and included patients with and without statin therapy. Several variations of discordance analysis were used including median-based, percentile-based, residual-based, and variance-based approaches.
RESULTS
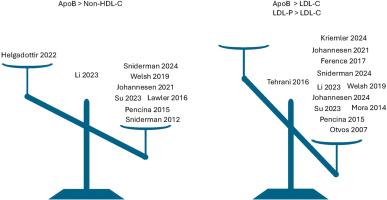
ApoB outperformed LDL-C in 9 of 9 studies whereas LDL P was superior to LDL-C in 2 of 3 comparisons. In 1 study, non-HDL-C was superior to apoB, in 1 study apoB and non-HDL-C were equivalent, whereas in 7 studies, apoB, overall, was a significantly more accurate marker of atherosclerotic cardiovascular disease risk than non-HDL-C.
CONCLUSION
Discordance analysis provides robust evidence that apoB is a more accurate marker of cardiovascular risk than either LDL-C or non-HDL-C, notwithstanding these variables are highly intercorrelated. Thus, neither LDL-C nor non-HDL-C are adequate clinical surrogates for apoB. Accordingly, apoB should be the primary measure in clinical care to estimate the cardiovascular risk attributable to the apoB lipoproteins and the adequacy of lipid-lowering therapy to reduce this risk.
载脂蛋白、LDL-C和非hdl - c作为心血管风险的标志。
背景:传统的统计方法不能用于比较低密度脂蛋白胆固醇(LDL-C)、非高密度脂蛋白胆固醇(non-HDL-C)和载脂蛋白B (apoB)等高度相关的变量。不一致分析是为了克服这一限制而设计的,方法是创建两个标记的预测不同的组。目的:本系统综述收集了比较LDL- c和非hdl - c与LDL颗粒数(LDL P)或载脂蛋白ob作为动脉粥样硬化疾病风险标志物的预测能力的所有不一致研究,以确定哪一种是最准确的心血管风险标志物。方法:PubMed检索于2024年9月30日完成,确定了15项研究,涉及593,354名参与者。这些研究涵盖了不同的人群,包括接受和未接受他汀类药物治疗的患者。使用了几种不同的不一致分析方法,包括基于中位数的方法、基于百分位数的方法、基于残差的方法和基于方差的方法。结果:ApoB在9 / 9的研究中优于LDL- c,而LDL- P在3 / 2的比较中优于LDL- c。在1项研究中,非hdl - c优于载脂蛋白ob,在1项研究中,载脂蛋白ob与非hdl - c相当,而在7项研究中,载脂蛋白ob总体上比非hdl - c更准确地标志着动脉粥样硬化性心血管疾病的风险。结论:不一致分析提供了强有力的证据,证明载脂蛋白ob是比LDL-C或非hdl - c更准确的心血管风险标志物,尽管这些变量高度相关。因此,LDL-C和非hdl - c都不能作为载脂蛋白b的临床替代品。因此,载脂蛋白ob应该是临床护理中评估由载脂蛋白ob引起的心血管风险和降脂治疗是否足够以降低这种风险的主要指标。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
7.00
自引率
6.80%
发文量
209
审稿时长
49 days
期刊介绍:
Because the scope of clinical lipidology is broad, the topics addressed by the Journal are equally diverse. Typical articles explore lipidology as it is practiced in the treatment setting, recent developments in pharmacological research, reports of treatment and trials, case studies, the impact of lifestyle modification, and similar academic material of interest to the practitioner.
Sections of Journal of clinical lipidology will address pioneering studies and the clinicians who conduct them, case studies, ethical standards and conduct, professional guidance such as ATP and NCEP, editorial commentary, letters from readers, National Lipid Association (NLA) news and upcoming event information, as well as abstracts from the NLA annual scientific sessions and the scientific forums held by its chapters, when appropriate.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


